The infamous thoracic outlet syndrome. TOS is considered to be one of modern medicine’s most difficult issues, because of the complex and variable nature of its symptoms. It has potential to cause numerous types and areas of pain, such as neuralgia in the arms, chest, between the shoulder blades and in the back (figure 1), dizziness, brain fog, migraine, headaches, a feeling of being “heavy-headed”, etc.
The reason why the potential symptoms are all over the spectrum, is because it in addition to compression of the entire brachial plexus nerve network which innervates the arms as well as parts of the chest, neck and back, also may compress the subclavian artery & vein. A branch of the subclavian artery include a key vessel, the vertebral artery. The VA supplies the brain with blood, and is therefore especially important to assess for symptoms of vertebrobasilar insufficiency. In cases where the vertebral artery is not rotationally compromised, compression of the subclavian artery will still influence craniovascular hemodynamics, because reduction of flow to the arm will increase flow rates to the head via the carotid and vertebral arteries, as shown in our recent study (Larsen et al. 2020) and cause craniovascular hyperperfusion. It has also been shown that TOS may cause secondary dysautonomic symptoms both due to its influence on craniovascular blood supply but also due to its potential for concomitant affection of the sympathetic nerves that connect to the brachial plexus. This can cause a truly weird and confusing constellation of symptoms.
Despite more than 2600 references to TOS on pubmed, there is still wide controversy regarding TOS; no concrete diagnostic criteria have been established, and many practitioners claim that the whole problem is a fad which does not really exist. Below are some interesting quotes related to thoracic outlet syndrome.
Fig. 1

This article is concerned with thoracic outlet compression syndrome (TOCS), one of the most controversial subjects in medicine. It may also be the most underrated, overlooked, misdiagnosed, and probably the most important and difficult to manage peripheral nerve compression in the upper extremity. – Atasoy, 1996
This review was complicated by a lack of generally accepted diagnostic criteria for the diagnosis of TOS. Thoracic outlet syndrome is one of the most controversial diagnoses in clinical medicine. – Povlsen et al., 2014
Thoracic outlet syndrome (TOS) is controversial in terms of definition, anatomy, aetiology and treatment. – Redman & Robbs, 2015
Actually it [TOS] is not widely known and it is also a controversial issue for some physicians. Moreover, it is sometimes strongly denied by those who have not had the opportunity of identifying it as a disease or even when they have not dealt with TOS patients…. We are confronted with a disease that is commonly undiagnosed by the majority of physicians. – Silva & Selmonosky, 2011
The diagnosis of neurogenic TOS is more challenging because its symptoms of nerve compression are not unique – Sanders et al., 2008
Conversely, no valid standard diagnostic test is available for disputed neurogenic TOS, resulting in controversies in the frequency of TOS diagnosis – Hooper et al., 2010
Diagnosis and treatment of thoracic outlet syndrome (TOS) involves neurologists, physiatrists, family physicians, orthopedic surgeons, vascular surgeons, thoracic surgeons, neurosurgeons and sometimes psychiatrists. – Köknel, 2005
The most commonly recommended interventions are strengthening and stretching of the shoulder girdle musculature.2,7,19,21 However, little agreement exists on which muscles need strengthening and which ones need lengthening.5 These types of exercises do not detail how they address functional TOS as a result of respiratory alterations and they do not aim to inhibit muscle.1,5,19 – Robey & Boyle, 2009
Neurogenic thoracic outlet syndrome (NTOS) is an oft-overlooked and obscure cause of shoulder pain that regularly presents to the office of shoulder surgeons and pain specialists. – Boezaart et al., 2010
Taking the research above into account, the reader can probably start to understand that it’s often very difficult to be properly diagnosed and treated if one has thoracic outlet syndrome. This article will shed light on what I consider a very effective approach to both diagnosis and treatment, that have cured thoracic outlet syndrome for most of our patients. Be aware though, that the actual treatment is a demanding procedure that will have to be managed through cooperation with a qualified therapist.
DISCLAIMER: This article is written for educational purposes only
Causes and consequences
The name thoracic outlet syndrome suggests chronic irritation (compression) of the brachial plexus and the subclavian vessels, as mentioned initially. “Thoracic” means region of the thorax (chest), and “outlet” is self explanatory. Why do they become irritated or compromised? Due to continuous compression within spaces that the nerves and vessels pass through. The cause of the compression is mainly tightness of the surrounding muscles and clavicular depression, strangulating the thoracic outlet vascular and nervous structures.
It is generally accepted that TOS is caused by compression of brachial plexus elements or subclavian vessels in their passage from the cervical area toward the axilla and proximal arm either at the interscalene triangle, the costoclavicular triangle, or the subcoracoid space – Köknel, 2005
Fig. 2

In turn, the main cause of the the muscle tightness and clavicular depression, is a combination of stress, postural dysfunction and muscular derangement or injuries. Patients with hypermobility disorders are also, empirically, quite susceptible to the acquisition of TOS. This can be rooted in habits alone, or triggered by injuries such as a clavicular fracture (Moon Jib Yoo et al., 2009; Ishimaru et a., 2012; Connolly & Dehne, 1989), whiplash injury (Schenardi, 2005) or similar. Slouching of the neck (forward head posture) and shoulders (Vanti et al., 2007), belly-(only)-breathing (Simon & Travell, 1999), and lack of diverse movement will cause the scalenes that form the interscalene triangle of which the brachial plexus pass through, to inhibit/deactivate. This in turn may cause severe tightening of the scalenes, compressing all of the thoracic outlets’ structures and may thus (with potential) cause all of the formerly mentioned symptoms. Although, perhaps, a less popular topic, it must be stated that a lot of TOS cases develop secondary to stress (Scaer 2011, Korn 2021). PTSD, anxiety, OCD and similar problems tend to cause the patient to become very tense, “clench” and hyperventilate, which over time causes dysfunction of the scalenus and pectoralis minor muscles. If the patient additionally “pec clenches”, this can dramatically lower the scapulae and cause costoclavicular syndrome. It is important to be aware of how psychological factors lead to tension which can lead to TOS. It is also common to develop TOS secondary to neck injuries, as whipping or cervical impacts can damage the scalenii and cause gross deterioration. The this process is often gradual, and TOS can onset anywhere from days to months after the incidence, depending on the particularities of each case.
The (anterior and medial) scalenes are involved in many actions. They elevate the ribs during inspiration (inhalation), ipsilaterally rotate, cause lateral translation, laterally flex and forward flex (bend) the neck. In normal breathing patterns, the ribs and clavicle should elevate slightly during inspiration, and this is done in syncronization by the scalenes, trapezius and several other muscles. Severe slouching habits will inhibit this pattern as well as proper cervical (axial) rotation, causing degeneration of the involved muscles. In turn, severe inhibition of the scalenes will often develop over time.
Because the trapezius muscle holds the scapula and clavicle, the loss of optimal function of this muscle will cause chain reactions of muscular inhibition down the line (arm), creating the potential for several nervous and vascular entrapment points, such as the triangular interval in the posterior shoulder. This is especially important when there is pre-compression within the scalenes and costoclavicular passage, as this sensitize the whole nervous chain and make the distal branches more vulnerable to additional irritation.
Additionally, because the scalenes attach to the ribs, they may elevate the first rib, greatly increasing the potential of secondary compression between the 1st rib and the clavicle. The ribs are normally quite flexible, thus the ability for ribcage expansion during respiration. In TOS, the rib elevation caused by scalenus tightness also causes rib rigidity. In turn, depression of the clavicle now crushes the nerves rather than just mildly compressing them due to a give in the 1st rib. This sequence of occurrences accounts for the majority of symptoms seen in TOS.
Fig. 3 – Venstre utløp

The myth of mandated muscular “release”
The weaker a muscle gets, the tighter it will feel. The patient may feel like stretching a steel wire that won’t budge when stretching a weak and inhibited muscle. It may get better for an hour or so, but then comes back with a vengeance. … And sadly, most repeat this process over and over until the only choice left is surgery. I have also addressed this topic in my lumbar plexus compression syndrome article.
Fig. 4 – Stretching is NOT the solution to your problems!
Extreme muscular inhibition will cause severe abrasiveness and tightening, greatly increasing its potential of irritating / compressing nearby structures such as nerves and blood vessels. In my experience, it’s a great and even potentially dangerous myth to assume that these tight muscles are “over active” and mandate release. This will make them even weaker and even tighter, as they are exposed to a stress that they can not handle.
Garrick and Webb1 in their excellent book, Sports Injuries: Diagnosis and Management, state that a weak muscle is a tight muscle. Whenever a weak muscle is forced to work beyond its capacity, it will tighten and, therefore, be more subject to stress and strain. – Warren Hammer, 1990
Bluntly, the myth of stretching (releasing) is one of the main reasons why most therapists are not able to cure thoracic outlet syndrome (or other nervous compression issues of muscular origin, for that matter) with conservative measures. The muscles that entrap the nerves and vascular structures must be strengthened significantly, so that they no longer reflexively tighten due to the unduly stress they’re exposed to.
That said, I can understand why people still do it. The stretching makes the client feel better! While strengthening on the other hand, makes it feel worse. And we want it to feel better, right? Wrong! The reason the strengthening makes it feel worse, is because the muscles are so utterly weak that any stimulus will cause exacerbation of the symptoms. They have minimal work capacity, which is why they severely tighten and irritate the surrounding nervous structures. The only way (that I know of) to deal with this, is slowly rehabbing the muscles by strengthening them steadily and easily over time.
Here’s an ultrasound image of a patient’s scalenes, clearly showing atrophy (degeneration w. fatty infiltration) of the muscle, especially the anterior scalene. Massaging such extremely weakened muscles will only exacerbate the situation. Note the difference in echogenicity between the sternocleidomastoid (scm) and scalenes (white structures = fat; the muscle should be relatively dark).
Fig. x
To systematically evaluate the muscles’ functions, it’s necessary to a testing tool. Such a tool is manual muscle testing (MMT), palpation, and strengthening exercises which are specific to the point of entrapment. I recommend David Weinstock’s book “Neurokinetic Therapy”, as it demonstrates the MMT tests well.
I have three rules that need to be fulfilled before I decide to release a muscle. If the muscle in question fits all of these rules, it’s probably safe to release. These “safe” (read: relatively healthy) muscles are usually not relevant to the patient’s complaint, in my personal experience, which is why I don’t perform releases all that often (many may, of course, disagree with this).
- The respective muscle is thick (hypertrophied)
- It has a high muscle tone (contractile status when resting)
- Tests very strong on a muscle test or with strength testing.
Beware that painful muscles tend to be weak, not strong.
Identification and correction
So far, the key points that we have talked about are:
- The importance of proper cervical and clavicular posture, and breathing patterns
- That the main compression occurs in the interscalene triangle, a well as the costoclavicular passage. The latter being the most sinister compression site.
- That the muscles causing the entrapment are usually extremely weak, and not over-active
It is absolutely critical to establish proper breathing habits, clavicular resting position and cervical posture, in order to resolve thoracic outlet syndrome. Supplementary, strengthening of all the involved inhibited structures should take place. Let us now go into detail about the underlying causes of all of these elements, and how they can be corrected.
Swayback posture (SBP)
Swayback posture is the most common stabilisation strategy I see utilised by clients with thoracic outlet syndrome. When the pelvis is tucked down and in (posterior pelvic tilt, lumbosacral flexion), it causes a shift in the body’s gravitational points so that the mid back hyperextends and the shoulders and head comes forward. It is almost impossible for a client to change their head and shoulder postural habits without addressing the root cause of it all, namely the pelvic tucking and thoracolumbar hinging. Additionally the pelvic tucking and forward head posture may cause breathing dysfunction, as it causes gripping of the abdominal muscles, making it hard to breathe diaphragmatically, and because it depresses the clavicle (as mentioned earlier).
I have written extensively about the topic of correcting swayback posture numerous times in my other norwegian articles, but also in this lower back article in english. Therefore it will not be elaborated further in this article, but it is paramount that the reader understands the chain reactions of pelvic misalignment on the head, neck and shoulders. And, of course its relation to breathing dysfunction.
Fig. 5

Spotting forward head posture is not difficult, but spotting clavicular and scapular misalignment on the other hand is often missed even by experienced therapists. As I have said already, the key to solving forward head posture is correcting pelvic and thoracic alignment. We will have a closer look on clavicular and scapular misalignment patterns, and how it can be identified and corrected shortly. But first, some elaboration with regards to swayback posture and breathing dysfunction is necessary.
How to correct your posture:
SBP and breathing
As we have already seen, SBP will affect our breathing strategy. Hanging forward with the head and slouching with the shoulders will inhibit the scalenes’ ability to elevate the ribs during inspiration, exacerbating the dysfunction.
To assess breathing, lie down comfortably on the back and evaluate whether or not there is adequate thoracic vertical expansion during moderate breathing intensity. Often, a very reduced vertical expansion will be noted. This can also be compared to standing up. A 70/30-ish percent expansion of the abdomen vs thorax is a well-balanced way to go, in my experience. To help this, it will be beneficial to strengthen the muscles that assist in thoracic inspiration: The sternocleidomastoid, scalenes, (and sometimes the pectoralis minor, but this will absolutely require proper scapular stability first)
Fig. 6

Many breathing “experts” claim that diaphragmatic (belly)-breathing is the ultimate cure to virtually anything. Ok, I am exaggerating a little, and I agree that diaphragmatic breathing ability is important, but teaching the client to reduce thoracic expansion may often lead to detrimental consequences (I learned this the hard way!). Thoracic expansion is normal, and abdominal expansion is normal. We need both.
So, in addition to the strengthening work that was mentioned above, we will of course need to work directly on our breathing habits. First, make sure that the clavicle is properly positioned (read more on that below). Then, try to make the thorax and abdomen expand in all 360 degrees as you inhale, getting into a calm rhythm of balanced respiration. If this is too difficult for you, either find a coach or work solely on thoracic vertical expansion, as this is most important element for resolving TOS. Remember that the clavicle should elevate gently as you breathe in, and gently depress as you breathe out. This cycle will need to be practiced over and over until it feels more normal or occurs automatically.
Beware that normalization of breathing should be reintroduced slowly, often over the course of years, in patients with TOS, especially in those whom symptoms are severe. The scalene muscles are very vulnerable in this patient group, and it is important to understand that imposing thousands of daily repetitions (breathing) after years of being dormant, can cause extreme flareup and worsening of symptoms. I have seen examples of this, mainly in “type A”, extremely motivated patients, overloading the scalenes to the extent of ruining the conservative treatment and unable to recover, even after months, and ending up needing surgical release. The takeaway is therefore to very gradually reintroduce chest breathing and to closely monitor your symptoms during this period to avoid progressive overloading and inflammation of the scalenes.
Proper scapular / clavicular resting position
The scapula should be located between the T2 and T7 vertebrae, with its superior angle levelled with T2 on the longitudinal line. This may however be cheated, by anteriorly rotating the scapula, which is a main trait when in slouching shoulders. Thus it is very important to be aware that the scapula should also be in mild upward and posterior rotation while positioned in height with T2 & T7. Most of the time, however, the scapula is so depressed that even with anterior rotation it will not be in line with T2, such as with the person in the picture below.
A typical TOS patient will often present with similar scapular resting position, as many studies (cited below) also show. The superior scapular angle is significantly inferior (lower than) the T2 vertebrae, and they rest in considerable anterior and downward rotation. Scapular depression and anterior tilt will cause the clavicle to jam into the brachial plexus and subclavian vessels, compressing them. Additionally, (as mentioned) inhibition of normal breathing patterns, cervical posture and rotation. A terrible combination that’s almost always found present in clients with thoracic outlet syndrome.
These patients are often cued by their therapist to pull the shoulders “back and down”, but this is very harmful and must never be done, as it causes compression of the costoclavicular space, and may result in nerve damage. Please consider that “back and down” is a provocative (orthopaedic) test for costoclavicular space syndrome (Magee, DJ. Orthopedic physical assessment, 2014).
Fig. 7

Regardless of what you have heard, no amount of strengthening will solve this problem. It’s rooted in habits, and must be corrected primarily by habitual changes. In practice that means relearning proper scapular resting position, by raising them into the proper height and rotational alignment and staying there. It’s hard work, but well worth it. Don’t get me wrong though; strengthening work is important. It’s just much less important than optimization of habits. I’ve written more about the scapular positioning topic in this shoulder pain article.
Optimal resting position should look something like the picture below. Ignore the muscle size, it is not important nor a criteria for proper positioning. However; the trapezius is clearly active, holding the scapula in proper height while also upwardly & posteriorly rotating it. This will ensure that the clavicle rests above the thoracic outlet, instead of crushing into it.
Fig. 8

Why you should NEVER pull the shoulders “back and down”
How to correct improper scapular and cervical positions:
Below are some relevant citations.
In our experience, droopy shoulder syndrome has accounted for most cases of thoracic outlet syndrome but is largely unrecognized by physicians. Recognition of this syndrome should lead to a better understanding of the underlying pathophysiology and prevent unnecessary surgery. – Swift & Nichols, 1984
Here’s a large quote collection from Watson et al., 2010 regarding the scapula’s relation to thoracic outlet syndrome. A great article that’s worth reading.
Thoracic outlet syndrome (TOS) is a symptom complex attributed to compression of the nerves and vessels as they exit the thoracic outlet. Classified into several sub-types, conservative management is generally recommended as the first stage treatment in favor of surgical intervention. In cases where postural deviations contribute substantially to compression of the thoracic outlet, the rehabilitation approach outlined in this masterclass will provide the clinician with appropriate management strategies to help decompress the outlet. The main component of the rehabilitation program is the graded restoration of scapula control, movement, and positioning at rest and through movement.
The conservative physiotherapy regimen outlined in this article will be suitable for patients presenting with TOS where there is a strong postural contribution to their symptoms. In particular, in cases of TOS where the scapula mechanics are poor and the patient presents with the dropped shoulder condition (scapula depressed and/or downwardly rotated, and/or anteriorly tilted) (Ranney,1996).
Many forms of scapula asymmetry may well exist in TOS populations, but in the limited research that has been done, scapula or shoulder girdle depression or “drooping” has been consistently observed (Kenny et al., 1993; Walsh, 1994; Pascarelli and Hsu, 2001; Skandalakis and Mirilas, 2001). Scapula depression will lead to
Scapula depression will lead to an alteration of the anatomical alignment of the structures in both the cervical and thoracic outlet (Telford and Mottershead, 1948; Kai et al., 2001; Skandalakis and Mirilas, 2001) (Fig. 2). It may potentially lead to tractional stress being placed on the nerve, vascular and muscular elements as well as compression as the clavicle descends closer towards either the first rib or any other bony element present. Elevation of the shoulder girdle can alleviate these stressors and potentially lead to “decompressing” the thoracic outlet (Kitamura et al., 1995).
One of the consistent objective findings that we have observed and measured in cases of sTOS is that the scapula can be depressed at rest (Fig. 3) on the symptomatic side compared to the other side (in unilateral TOS) and to the normative data in cases of bilateral TOS (Kai et al., 2001). Increased anterior tilt of the scapula is also commonly identified in sTOS (Sucher, 1990; Aligne and Barral, 1992; Press and Young, 1994; Walsh, 1994) and it is frequently coupled clinically with increased downward rotation of the scapula. – Watson et al., 2010
Neurogenic TOS
The symptoms of TOS may greatly vary. They are not unique, and this is one of the main reasons why making a diagnosis is difficult. Many of the same clues are however often present, and this is what we need to use as a measure of probability. Initially, patients often present with pain between their shoulder blades via the dorsal scapular nerve, and, of course, neck pain. Ulnar neuralgia or paresthesia is also a common initial symptoms of TOS, as the C8 and T1 roots lie more susceptible for compression in the costoclavicular interval. As the disorder progresses, pain in the chest, face (cervical plexus co-affection) and full arm may develop. Sympathetic comorbidity such as tremors, Reynaud’s syndrome or causalgia may develop. Many patients also feel tightness of of, or a “lump” in the throat (globus hystericus), which is often misdiagnosed as a psychiatric symptom. Dyspnea (difficulty breathing) and pnealgia (painful respiration) is also relatively common in this patient group, as bilateral brachial plexopathy may impair the function of the phrenic nerve, although this is not well known.
Neurogenic TOS is very easy to trigger, and this is tremendously helpful while diagnosing and identifying nervous entrapment points down the branches of the brachial plexus. To do this, I use a pressure-testing “technique” as means of provocation. The concept is simple: Push into the entrapment point and see if it reproduces the pain. This is called a positive Tinel’s sign. If it does, this is a region that’ll need corrections. There are potential entrapment points all the way down the arms, in the route of the nervous branches. We will now look more closely on these, and how each branch can be addressed.
The tinel’s sign has been shown to have poor specificity in the literature, but because plexopathic problems are so controversial, there is not reason to rely on this. The Tinel’s sign is a very good indicator of entrapment. If it hurts, there is a problem. It should not hurt! A reason why surgeons require high specificity testing for TOS (although such does not exist) is simple: They do not want to operate unless clearly warranted. This understandable! However, with proper conservative treatment, such risks are not present, and we need to be so wary of false positives. If it hurts, we strengthen the muscle which is most likely to irritate the nerve. Risk free!
With regards to diagnosis of N-TOS, it has been shown that EMG, NCV and MR neurographies are not reliable diagnostic criteria (Tolson 2004, Passero 1994, Veilleux 1988, Aminoff 1988, Rousseff 2005, Kwee 2014) There have also been reports of EMGs only being positive when the patient is in certain positions (Fishman 2002), and reports that motor nerve NCVs have been negative while sensory segments positive (Machanic 2008). I have seen several patients with severe pain upon pressure to the interscalene triangle, positive myotome tests etc., who still did not have any findings upon EMG. The sensitivity of these tests are simply inadequate and should not be used to exclude pathology. They may be used to quantify the problem, once already implicated, however.
NCV can be prolonged by injury or simple extrinsic pressure against a nerve.41 NCV prolongation is especially seen in patients with long-standing NTOS that results in muscle atrophy.42 However, other articles have reported that NCV is often normal in patients with symptoms of NTOS.42,43
Somatosensory evoked potentials studies have been found useful in some reports.46,47 However, somatosensory evoked potential has also been criticized as nonspecific, nonlocalizing, and rarely abnormal.43,44,48
Findings showed denervation activity, increased mean action potential amplitude, and/or duration and reduced recruitment at maximum effort. However, there is still some question as to whether EMG is adequately sensitive to detect changes in NTOS patients with milder symptoms.42,45 – Sanders et al., 2008
Somatosensory evoked potentials (SEPs) are used in the diagnosis of thoracic outlet syndrome (TOS), even as an indication for surgery. The purpose of this study was to evaluate the use of SEPs in the diagnosis of TOS. Twenty-one patients (mean age, 37 years) with TOS and 23 control subjects (mean age, 34 years) were included. Somatosensory evoked potentials of median and ulnar nerves were measured bilaterally in patients in both a relaxed and arms-elevated provocative position. A three-way analysis of variance showed no significant difference between the interpeak latencies of the TOS and control groups (p = .352). Significant differences were found in testing positions (p = .0014) and nerve tested (p = .001) in both groups. Therefore, this study suggests that SEPs are not helpful in the diagnosis of TOS. – Komanetsky et al., 1996
Fig. 9
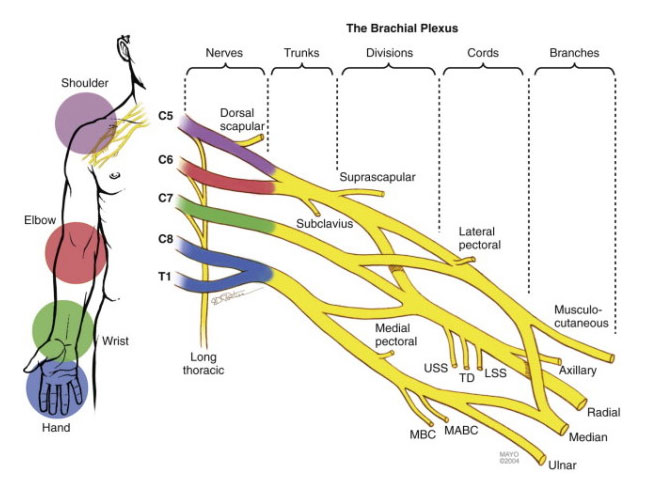
Brachial plexus compression sites
Compression directly to the brachial plexus is the most common driver of thoracic outlet syndrome. It is comprised of two main entrapment zones, which are the interscalene triangle and the costoclavicular passage.
The interscalene triangle is usually the main entrapment point (culprit), and will often stand for 60-80% of the patients’ symptoms. When scalenes are very very tight, they also elevate the first rib, furtherly reducing the space between the rib and the clavicle, increasing the potential for compression within the costoclavicular passage. Compressive forces within the interscalene triangle will affect all of the thoracic outlet’s structures and may thus cause all of the symptoms that were mentioned in the beginning of this article.
Fig. 10

To evaluate the scalenes’ involvement, the therapist pushes the thumb into the brachial plexus, in the middle of the distal anterior and middle scalene fibers. Start light and gradually go hard(er), to see if the symptoms reproduce. This is called the Morley’s test (Sanders 2007, Laulan 2011). You need to push directly into the brachial plexus. If you miss the right spot on a patient with TOS, you’ll get a false negative. It’s a generally a good idea to move the thumb around a little to make sure that your test results are accurate.
Some may argue that pressure directly into a muscle that lies on top of a nerve, always will cause nervous symptoms, but this is NOT true. I use these tests almost every day, and they will show up negative if there is not nervous irritation in the region you’re testing.
If the pressure reproduce the symptoms, you’ll want to muscle test (MMT) the surrounding muscles. For the anterior scalene, resist above the eyebrow while client the head toward the shoulder. Medial scalene, resist at temple while client moves head toward the shoulder. Watch out for clenching of the jaw, breath-holding, etc, as the body would try to cheat and use any synergist rather than the scalenes to protect the already irritated brachial plexus from the activation of the scalenes.
If the pressure test reproduced the pain but the scalenes test strong, most of the time that means the test is skewed. MMT is a skill that takes time to develop, but is extremely useful when you get good at it. Tell the patient to relax and to resist your pressure naturally, without engaging all the muscles of the neck. The point here is to assess the specific muscles’ functions, not to “win”.
Fig. 11-12 – Scalenus anterior (left) & medius (right) MMT


Here are the exercises for scalene strengthening. Make sure that the person doing it starts very, very easy. Going on hard on these exercises may trigger tremendous pain and significant worsening of the symptoms. It should get a little worse as the scalenes are worked, but not cause excruciating pain. 5 reps for 1-2 sets twice per week is usually a safe start.
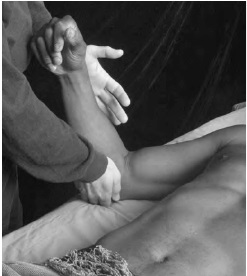
To check for entrapment within the costoclavicular passage, I use a clavicular depression test. Either with the patient sitting, or supine, the therapist strongly depresses the shoulder manually to see if this will reproduce the pain. Again, a strong pressure will usually be required. The patient can also pull their shoulders back and down. Hold it for at least 30 seconds, and look for tingling or frank pain in your arm, hand, chest, neck or scapula. If the test reproduce the pain, which it often will if the scalenes are affected, this means that the clavicle is too posturally depressed and is irritating the thoracic outlet within the costoclavicular passage. This test can also be falsely negative if there is numbness of the nerves (a consequence of long term compression), so don’t rely fully on it.
As I’ve said many times now, this is a postural and breathing related issue. The trapezius may be strengthened by performing shrugs or similar exercises, but the habitual changes are what will yield long lasting results in this case. Raising the shoulders slightly in posture (and staying there) will decompress the thoracic outlet. Optimization of thoracic vs. diaphragmatic breathing balance will also stimulate the scalenes, as mentioned earlier.
Fig. 13

If the costoclavicular space (CCS) is compromised, which is more serious than muscular entrapment (as bones will be compressing the nerves, as opposed to myofascial irritation), there will usually be subsequent myotome weakness. Myotome testing is therefore important to do on these patients, to evaluate the degree of compression. Most commonly, the inferior trunk of the brachial plexus will be affected. This is because it lies most anteriorly of the trunks, making it more susceptible to compression. Inferior trunk compression will usually cause weakness of the 5th finger (ulnar nerve), and sometimes triceps and axillary nerves (radial and axillary nerves). Sometimes the middle trunk may be affected as well, which causes weakness of the biceps (musculocutaneous nerve). The median nerve is rarely affected by costoclavicular space compression (superior trunk).
Myotome tests:
- 2nd finger opposition – Median nerve – Superior trunk
- Biceps – Musculocutaneous nerve – Middle trunk
- Lateral deltoid – Axillary nerve – Inferior trunk, middle trunk
- Triceps – Radial nerve – Inferior trunk
- 5th finger opposition – Inferior trunk
- Finger abduction – Inferior trunk
If significant weakness is discovered, it is an utmost high priority to decompress the CCS.
Back to Tinel’s sign. You can also push into the pectoralis minor to see whether it reproduce any symptoms or not. This test, however, is not all that useful. The subcoracoid space-compression (beneath pectoralis minor) is rarely a big player in the dysfunction, and will almost always resolve on its own when the posture, scalenes and clavicle have been corrected.
The retropectoralis minor space is a very rare potential site of compression. – Demondion et al., 2006
As I mentioned earlier, postural dysfunction will cause scapular instability. This, in turn, will often cause a chain reaction of inhibition down the lines of the arm, as these structures mostly depend on the stability of the scapula to be able to generate force safely. It’s very important to also address these secondary sites of compression. What you’ll likely come to notice is that “carpal tunnel syndrome” and similar issues are often just a secondary TOS-symptom. Let’s have a closer look at these secondary sites of compression, and how they can be assessed and corrected. These principles also apply if TOS is negative, it is just not as common.
The cervical plexus
Cervical plexus entrapment is a very little known, but somewhat common comorbidity in thoracic outlet syndrome. The cervical plexus is comprised of C1-4 nerve roots, and mainly carry sensory functions. The cervical plexus itself can become entrapped between the middle scalene and levator scapula muscles, and in these cases, symptoms will usually trigger either with [excessive] stimulation of the scalenus or levator scapula. This can be hyperventilation, heavy carrying and working overhead, or especially horizontal pushing. The cervical plexus can also be symptomatic in the absence of direct stress, meaning that its symptoms are mainly invoked by stress exerted on the brahcial plexus.
Symptoms of cervical plexus entrapment are neck and throat tightness, ear pain, mastoidal pain, occipital neuralgia (may implicate any of the three different occipital nerves: The greater occipital, lesser occipital and 3rd occipital nerves), supraclavicular pain, and of course, generalized neck pain. The suboccipital symptoms in TOS are usually vascular, and as such, hypertensive migraines. But some patients suffer from legitimate neurogenic suboccipital symptoms in TOS, and these will respond favorably to a nerve block, whereas the vasculogenic one will not. In neurogenic cases, one will usually also be able to elicit a Tinel’s sign with sustained pressure directly applied to the nerve, or see other associated symptoms such as hyperesthesia or numbness in the region of innervation.
The radial & axillary nerve compression sites
The main compression site for the radial nerve, is within the triangular interval and between the fibers of the supinator muscle. To test for affection, squeeze your thumb into the interval in the posterior armpit, and/or into the supinator muscle. If pain is reproduced, you can evaluate the muscles that surround the nerve’s function by using palpation and MMT. Weakness and hypotonus of the teres minor, lateral & long heads of the tricep will usually be present for the posterior shoulder. It’s virtually always appropriate to initiate a strengthening protocol on these structures.
Fig. 14

The axillary nerve passes through the quadrangular interval, and will usually be compressed between the teres minor and teres major. As usual, squeeze into the interval with your thumb to see whether the symptoms reproduce. If they do, you can MMT the teres major and minor, or just initiate a strengthening protocol right away as they’ll test weak anyway. Strong, healthy muscles are rarely responsible for neuralgia.
Fig. 15

As explained, the supinator and triangular interval are by far the most common regions of radial nerve compression. The two most useful MMTs are provided here, for the teres minor and supinator muscles. To test the supinator, client resist the therapist’s attempt to pronate his wrist. For the teres minor, the same principle, but by resisting internal humeral rotation.
Fig. 16-17 – Supinator MMT (left), Teres minor MMT (right)

Exercise for the lateral rotators
Exercise for the supinator muscle
The median nerve compression sites
Most of the same principles of both identification and correction apply to the median nerve. The entrapment points of the median nerve are underneath the pronator teres muscle, and within the carpal tunnel.
The carpal tunnel is a little different than the rest of the compression points in this article. Eleven tendons pass through the CT, and even slight hypertrophy of these will greatly reduce the space within the tunnel. Flexor dominance will lead to hypertrophy, and may thus lead to strangulation of the median nerve within the carpal tunnel. Stretching the finger flexors followed by strengthening of the finger and wrist extensors may be a very beneficial and rewarding protocol.
Fig. 18
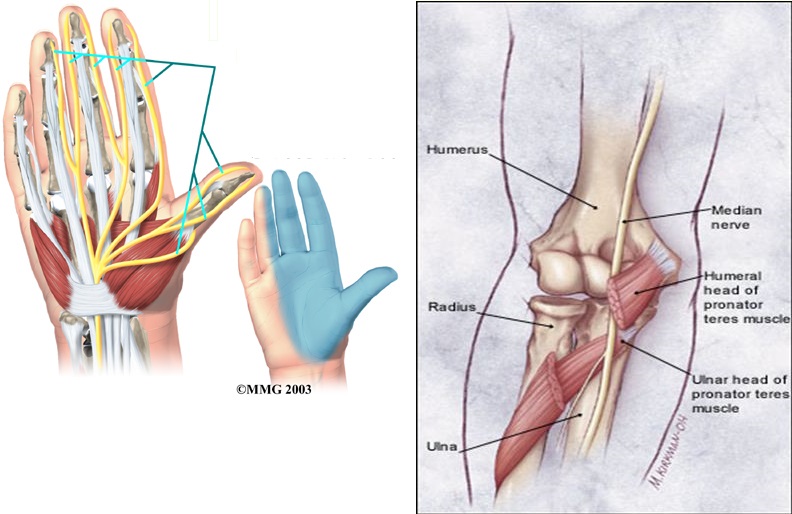
Pronator teres “syndrome”. Squeeze into the pronator teres and see whether it reproduces median neuralgia. If it does, MMT it by having the client resist your attempt to supinate their wrist. If it’s weak, strengthen it with the exercise provided in the video about wrist supination and pronation, further up.
Fig. 19 – MMT for the pronator teres

The musculocutaneous nerve compression sites
Musculucutaneous nerve compression often cause misleading symptoms in the lateral arm, mimicking radial nerve pain. It’s actually quite common, but it took me some time to figure this out. The nerve passes through the coracobrachialis, and then between the biceps and brachialis muscles. The patient will often lack significant medial humeral rotation when the MCN is affected, often appearing to be a mobility problem at first.
To evaluate compression between the biceps, squeeze into the distal biceps. If symptoms reproduce, test the biceps and brachialis muscles. Commonly I find that the biceps are weak and brachialis is strong, in which you may release the brachialis and strengthen the biceps (remember to force supination during elbow flexion). No absolutes, though.
Fig. 20

The same assessment protocol applies to the coracobrachialis. Elevate the arm and squeeze into the musculocutaneous nerve. If this reproduces the pain, test the muscle. If it’s weak, and it usually is, strengthen it.
Fig. 21 – Coracobrachialis MMT

Myotome tests
Nerve compression neuropathy may lead to muscle weakness. Such weakness in the sequela of neuropathy is called a positive myotome test. The best way to evaluate myotomes are to look for relative weaknesses, as utter paralyzation is usually not present. Weakness is usually not a cause of muscular entrapment, but rather of costoclavicular space compression (i.e. osseous compression of the brachial plexus).
The inferior trunk of the brachial plexus lies most susceptible placed within the costoclavicular space, i.e. more forward. With depression of the scapulae, this may cause weakness of the fifth finger and finger abduction (C8 and T1 nerve roots). Thus relative weakness of the fifth finger with regards to opposition and abduction (Selmonosky 1981, 2002, 2008) is a good criteria for detection of TOS. Such weakness indicates inferior trunk compression unless there is C8 or T1 radiculopathy (disc herniation).
As the problem progresses, weakness of the triceps and wrist flexors (radial nerve, C7 nerve root) and medial deltoid (C5 nerve root) may occur. Usually the median nerve is not affected (weakness of the 1st finger). There may sometimes be weakness of the biceps (musculocutaneous nerve, C5-6 nerve roots).
Compare the affected and unaffected sides to evaluate relative weakness and thus estimate degree of weakness sequelar to nerve compression. As mentioned, if there is weakness, the most common cause is costoclavicular space compression (depressed scapulae and/or scapular dyskinesis).
Fig. 22 – Source: tos-syndrome.com
The ulnar nerve compression sites
The ulnar nerve is often just a side effect from the compression in the thoracic outlet. However it may be slightly compressed beneath the flexor carpi ulnaris muscle, and within the arcade of struthers which is a passage between the medial triceps and medial intermuscular septum. When the medial triceps is weak, the struther’s passage tightens, often causing the typical neuralgic symptoms of the meidal elbow and into the little- and ring fingers.
The same protocol applies: Test the medial tricep and FCU. If they’re weak, strengthen them by performing elbow extensions in slight lateral humeral rotation and wrist flexion with ulnar deviation. The medial tricep can be tested by having the patient resist elbow flexion while in slight lateral humeral rotation. The FCU, by having the patient resist wrist extension by flexing it with ulnar deviation.
Fig. 22

Once in a while, the pressure test will be positive but the MMT truly negative. This generally means that the compression is stemming from another structure, and that the area that you’re working on is not that important. No absolutes, though. Use MMT, palpation and provocative pressure tests to find the answers.
Arterial / Vascular TOS
Arterial thoracic outlet syndrome is thought to be very rare. It has infact been estimated that approximately 95% of the thoracic outlet syndrome cases are related to neurogenic symptoms (Wilbourn et al., 1990). But, how reliable is this estimate? First of all, neurogenic TOS is in general misdiagnosed, overlooked, etc even though it is the most easily triggered type of pain. Arterial TOS is much more subtle, and may mimic many other issues. It is therefore extremely difficult to quantify its involvement and thus, in my view, highly unlikely that this estimate is reliable.
The most common symptoms of arterial and/or venous TOS are:
- Dizziness / vertigo
- Suboccipital, or mastoidal pain and pressure
- Migraine and/or headaches
- Cold hands and arms
- Feeling “heavy-headed” or as if wearing a tight helmet
- Difficult to concentrate
- Fatigue
- More rare; ischemia of the arm or hand
- Also rare; swelling
Most of these symptoms may have several other potential causes, which is why you need to do a probability estimate of whether thoracic outlet compression may be involved or not. One factor that often holds true, is visible increase of pressure in the external jugular vein. This is almost always caused by tightness of the SCM and scalenes, and/or depression of the clavicle (we now know that these two often go hand in hand), as it compresses the subclavian artery and thus compromises these structures. You can also have the patient elevate the arm, then evaluate whether or not the radial pulse diminishes, which would indicate compromisation of blood flow and thus also arterial TOS.
Fig. 23 – Source: tos-syndrome.com
Selmonosky (1981, 2002, 2008) describes a simple test for brachial ischemia or cyanosis which involves maximal elevation of the arms. The patient leaves the arms up for 1-2 minutes, and the therapist looks for a White hand sign (WHS), which implies cadaveric paleness of the affected hand, usually along with tiredness and/or pain. There may also be venous insufficiency, causing venous distention and purpuric skin color indicative of cyanosis.
Fig. 24

If the posture, breathing, and neurogenic pressure-testing all have indications of dysfunction, and of course that the patient presents with additional vascular symptoms, they may very well be caused by vascular thoracic outlet compression. I noticed this connection especially as some clients were complaining of dizziness and migraine-like symptoms during strengthening regimes for the scalenes.
Research has demonstrated a connection between compression of the subclavian artery and compromise of the vertebral artery, an artery that supplies the posterior brain with blood. Here are some interesting quotes.
Thoracic Outlet Syndrome (TOS) causes dizziness because of positional compression of the vertebral artery with resultant symptoms of vertebrobasilary insufficiency. Compression of 7,C8,and T1 nerves fibers is responsible for the neck pain. – Selmonosky, 2007
The cases of 17 patients with vertigo, tinnitus, deafness, supraclavicular bruit, and a diminished radial pulse are reported. All the patients had an anomalous vertebral artery. All had subclavian-vertebral arteriograms preoperatively. Each patient showed an anomaly of the vertebral artery system which allowed intermittent compression of either the origin or cervical course of the artery. The compression was usually aggravated by rotation or hyperextension of the neck. In most cases, the vertebral artery arose at the level of the thyrocervical trunk and the compression was relieved by section of the scalenus anticus muscle and by division of the inferior thyroid artery. – Powers et al., 1961
We report a patient who developed occasional vertigo when turning his head to the right side. Occlusion of the right vertebral artery occurred at the narrowed “scalenovertebral angle” with this rotational head movement. This triangular tunnel consisted of the hypertrophied ligament of the longus colli muscle and the anterior scalene muscle. – Kojima et al., 1985
Rotation-induced vertebrobasilar artery hypoperfusion causes transient ischemic attacks (TIAs), affecting the cerebellum, brainstem and spinal cord. When these symptoms occur transiently due to head movement, compression of the vertebral artery by an extraluminal lesion should be suspected. Cervical spondylotic spurs and anterior scalene muscle or deep cervical fascia are among the factors which can compress the vertebral artery. – Dadsetan & Skerhut, 1989
Rotational positioning of the head showed vertebral obstruction in one direction, and unobstructed filling of the vessel when the head was turned to the opposite side. Fifteen patients showed rotational vertebral artery occlusion. The site of obstruction occurred at the origin of the vertebralartery or cephalad to the level of C5. Two patients had bilateral fascial band obstruction, one patient had left only, and the remaining 10 were obstructed on the right side. An anterior scalenotomy was done with preservation of the phrenic nerve. We were more impressed with the deep cervical fascia as the cause of intermittent rotational obstruction rather than the anterior scalene muscle. Only two patients showed unequivocal poststenotic dilatation as evidence of severe anterior scalene muscle compression. The obstructing extra-luminal fascia was quite dense, fibrotic and often completely encircling the artery. – Hardin & Poser, 1963
Subclavian steal symptoms presents secondary to arterial insufficiency, created by a retrograde flow that “steals” blood from the brain circulation, more specifically from the basilar artery via the vertebral artery. Classically it presents with neurological symptoms from the posterior brain and cerebellum [4,6]. Decreased flow over the basilar artery gives rise to symptoms like lightheadedness, ataxia, vertigo, dizziness, confusion, headache, nystagmus, hearing loss, presyncope and syncope, visual disturbances, focal seizures, and in extremely rare cases, death [6–10]. However the vast majority of patients are asymptomatic and rarely require any intervention [3,5,11]. – Alcocer et al., 2013
This article describes migraine without aura since childhood in a patient with bilateral cervical ribs. In addition to usual migraine triggers, symptoms were triggered by neck extension and by arm abduction and external rotation; paresthesias and pain preceded migraine triggered by arm and neck movement. Suspected thoracic outlet syndrome was confirmed by high-resolution bilateral magnetic resonance imaging (MRI) and magnetic resonance angiography (MRA) of the brachial plexus. An unsuspected aberrant right subclavian artery was compressed within the scalene triangle. Left scalenectomy and rib resection confirmed the MRI and MRA findings; the scalene triangle contents were decompressed, and migraine symptoms subsequently resolved. – Saxton et al., 1999
Thoracic outlet syndrome (TOS) refers to the compression of the neurovascular bundle within the thoracic outlet. Cases are classified by primary etiology-arterial, neurogenic, or venous. In addition to the typical symptoms of arm swelling and paresthesias, headaches have been reported as a potential symptom of TOS. In this report, we describe a patient with debilitating migraines, which were consistently preceded by unilateral arm swelling. Resolution of symptoms occurred only after thoracic outlet decompression. Patients with migraines and concomitant swelling and/or paresthesias, especially related to provocative arm maneuvers, should be considered a possible atypical presentation of TOS and evaluated in more detail. – Chahwala et al., 2017
It is also noteworthy that the hypertrophied and contracted anterior scalenus muscle exerts a strong although intermittent compression of the vertebral artery, causing in severe TOS diverse symptoms that are very characteristic of vertebrobasilary insufficiency. – Silva & Selmonosky, 2011
Reports of transient blindness resulting from this condition are even more rare. The authors describe the case of a middle-aged woman who presented with transient blindness when she turned her head excessively to the left. She also exhibited other less severe brainstem symptoms. Arteriography demonstrated occlusion of the left vertebral artery only when her head was rotated to the left. Surgical exploration revealed entrapment of the left vertebral artery by a tight anterior scalene muscle, release of which resulted in complete resolution of her symptoms. – Sell et al., 1994
Triggering the symptoms may be a little challenging. If it’s headaches, try to rotate and flex the head contralaterally while in cervical extension and lying supine, to tighten the scalenes around the thoracic outlet. The therapist may also force the clavicle caudally. Hold this for a few minutes and have the patient stand up. Dizzy? Drowsy eyed? Heavy-headed? If any relevant symptoms appear after the provocation, that is a strong indication that there are vascular implications in the given case of thoracic outlet syndrome.
If symptoms appear within 15-30 seconds while still lying on the table, this may indicate vertebral artery dissection (VAD). This is a potential emergency, and must be screened and/or treated as soon as possible at a hospital. Read more about VAD HERE.
Fig. 24
The approach of corrections remain the same, however. We want a posture that remains the head, cervical spine and clavicle in optimal position. Breathing habits will need to be worked on, especially with regards to thoracic vertical expansion during inhalation. Additionally, the scalenes and sternocleidomastoid will need strengthening, along with any relevant compression you may find in the extremities.
Here’s a patient with ipsilateral migraine and facial numbness. In normal position, there is nice normal flow within the vertebral artery, with a strong signal. Because ultrasound is not quantitative, meaning that it can not reliably quantify blood volume, it is generally used for qualitative assessments, meaning that evaluation of flow speeds and waveforms are used to estimate whether or not the flow is “normal”. The problem is that the reference ranges for these scans are very wide, and it is very easy to get a false negative. Thus one needs to evaluate changes between the foraminal levels, as well as with rotation in both directions while in cervical extension.
Signal strength indicates the amount of blood that travels at the given speeds, and is thus quantitative. Did I not just say that ultrasound is not quantitative? Here’s the problem. Signal strength is very, very easily altered. Too much or too little gel, poor probe position or insonation angle, changed by gain levels, etc. Thus, one needs to keep the same insonation angle, depth, as well as gel amount, and MOST IMPORTANTLY keep the same gain setting when evaluating changes. Usually slight speed changes, but large signal changes are seen in patients with non-acute pathology, such as TOS-related migraines or similar.
Fig. x
Turned head to the right, i.e. in a position similar to that of DeKleyn’s (VAD) test shows significant loss of flow volume, indicated by obliteration of signal.
Fig. x
TOS may also lead to migraines in the absence of vertebral artery compression. Tightness (due to weakness) of the scalenus muscles will compress the subclavian artery, especially during ipsilateral rotation and extension of the neck. As the subclavian artery compresses, the blood that is supposed to enter the arm is forced to redirect into the head. In result, intermittent or sometimes even chronic hyperperfusion of the carotid and vertebral arteries may occur (Larsen et al. 2020). Carotid hyperperfusion syndrome is a phenomenon usually associated with carotid stent placement, i.e. in relation to surgical intervention of atherosclerosis. However, musculoskeletally induced hyperperfusion may also occur, as stated, if the inlet to the arm is obstructed (Larsen et al. 2020)
Similar to that of hypopefusion (flow deficit), hyperperfusion is also associated with migraines, headaches, dizziness, transient bell’s palsy, nausea, hemiplegia palsy and more (Adhiyaman 2007, Tehindrazanarivelo 1992, Coutts 2003, Sundt 1981).
TOS and autonomic dysfunction
Another very interesting aspect of thoracic outlet syndrome, though somewhat more rare, is its potential for autonomic nervous system irritation. The somatic nervous system and autonomic nervous system is interconnected through something called gray rami communicans. When the somatic nerves such as the brachial plexus are entrapped, the dysfunction may “bleed over” into the autonomic chains, just as a lumbar disc herniation may cause pain from the back down into the foot.
A relatively common symptom is chronic cough, but I’ve also seen chronic hiccups, increased heart rate upon cervical rotation, dry throat syndrome, clogged ears, tinnitus, burning tongue and even pseudoangina symptoms occur in some of these patients. I have also seen associations between autonomic irritation and atrial fibrillation. Because these nerves innervate virtually all organs in the body, it is difficult to list all the possible symptoms that could occur when they are irritated. See some interesting evidence below.
Fig. x
In neurogenic TOS, neurogenic symptoms occur in the upper extremity and may radiate to the shoulder, neck, and occipital regions if the upper trunk is involved; Raynaud phenomenon is frequently seen due to an overactive sympathetic nervous system, whose fibers run along the C8 and T1 nerves. – Aralasmak et al., 2010
Chest pain or pseudoangina can be caused by TOS. Dorsal sympathectomy is helpful for patients with sympathetic maintained pain syndrome or causalgia and patients with recurrent TOS symptoms who need a second procedure.
Compression of the sympathetic nerves in the thoracic outlet may occur alone or in combination with peripheral nerve and blood vessels. The sympathetics are intimately attached to the artery as well as adjacent to the bone. They may be compressed or irritated in primary or recurrent TOS. Atypical chest pain (pseudoangina) simulates cardiac pain (48). Major indications for dorsal sympathectomy include hyperhidrosis, Raynaud’s phenomenon or disease, causalgia, SMPS, reflex sympathetic dystrophy, and vascular insufficiency of the upper extremity.
To explain chest pain from TOS compression, it is important to remember there are at least two types of pain pathways in the arm: the commonly acknowledged (C5 to T1) somatic fibers, which transmit more superficial pain, and the afferent sympathetic nerve fibers, which transmit deeper painful stimuli. The cell bodies of the two types of neurons are situated in the dorsal root ganglia of the corresponding spinal segments. They synapse in the dorsal gray matter of the spinal cord, and the axons of the second-order neurons ascend in the spinal cord up to the brain. Compression of the superficial C8 to T1 cutaneous afferent fibers elicits stimuli that are transmitted to the brain and are recognized as integumentary pain or paresthesias in the ulnar nerve distribution. In contrast, compression of the predominantly deeper sensory fibers elicits impulses that are appreciated by the brain as deep pain originating in the arm or the chest wall, even if the source of the impulses is cardiac (referred pain). – Urschel & Kourlis, 2007
Cough attacks elicited by movement of the neck and right arm are reported in a patient who had sustained several shoulder injuries and who had an anterior scalenectomy. The coughing was accompanied by weakness in the right upper limb. At exploration, the phrenic nerve was found adhered to the brachial plexus. The cough attacks disappeared, and the weakness of the right upper limb improved somewhat after lysis of the adhesions between the phrenic nerve and the plexus and after external neurolysis of the upper, middle, and lower trunks. Postoperatively, the patient could elevate his right arm without coughing. – Yamagami et al., 1994
In this case report, we rendered a 22 year old woman with the diagnosis of neurogenic thoracic outlet syndrome. We have evaluated her symptoms of palpitation with Holter monitorization during Roos test before and after surgery where transaxillary first rib resection and scalenectomy were performed. Postoperatively she improved and the tachycardia resolved. We propose that stellate ganglion or postganglionic efferent sympathetic fibers forming the cardiac plexus are exposed to compression while Roos test is being performed. Due to this irritation, there can be an increase in the cardiac sympathetic activity. – Kaymak et al. 2004
Four patients with elevated creatine phosphokinase (CPK) values and recurrent chest pain were found to have thoracic outlet syndrome. This association of abnormal CPK levels and chest pain due to thoracic outlet syndrome has not been previously reported. Symptoms and CPK values improved with anti-inflammatory medications and/or proper posture instruction. It is proposed that CPK values become elevated by ischemic or neurologic compromise of muscles supplied by the subclavian artery or brachial plexus respectively. Accordingly, chest pain in the same dermatomal distribution as that of angina pectoris may be simulated by ischemic skeletal muscle. – Godfrey et al., 1983
Forty-four patients presenting with chest pain suggesting coronary artery disease had normal exercise stress tests and selective coronary angiography and subsequently were found to have an unsuspected thoracic outlet syndrome. Pathways of pain in angina pectoris and afferent stimuli originating from brachial plexus compression at the thoracic outlet stimulate the same autonomic and somatic spinal centers that induce referred pain to the chest wall and arm. – Urschel et al., 2010
There has been increasing evidence that dysfunction of the autonomic nervous system that encompasses the sympathetic, parasympathetic and intrinsic neural network is involved in the pathogenesis of AF (atrial fibrillation).
Sympathetic system may promote arrhythmia by increasing Ca2+ transient. Activated β-adrenergic signal pathways increase Ca2+entry and the spontaneous release of Ca2+ from sarcoplasmic reticulum (36). However, vagal stimulation or perfusion of ACh in experiments contributes to development of AF by heterogeneous shortening of action potential duration and refractory period. With vagal hyperactivity, the atrial repolarization is abbreviated by ACh-activated potassium current (IKACh) (37), and/or non-cholinergic and non-adrenergic neurotransmitters, such vasoactive intestinal polypeptide VIP (38). Furthermore, studies have demonstrated that the interaction between sympathetic and parasympathetic nervous systems in developing AF by recording nerve activities directly from stellate ganglia, and vagal nerve (39).
Parasympathetic stimulation has long been associated with increased propensity to AF (40,41). The onset of paroxysmal AF often may be preceded by evidence of increased vagal tone, especially in patients with lone AF who otherwise have structurally normal heart (29). – Xi & Cheng, 2015
Symathetically mediated atrial fibrillation is observed in the presence of any heart disease, the first effect of which is to provoke a vagal withdrawal. The role of the autonomic influences should be taken into consideration every time conventional antiarrhythmic treatment is insufficient. – Coumel, 1994
Pathways of pain in angina pectoris and afferent stimuli originating from brachial plexus compression at the thoracic outlet stimulate the same autonomic and somatic spinal centers that induce referred pain to the chest wall and arm. – Urschel et al., 2010
A 60-year-old man experienced arrhythmia when he turned his head to the left and had these symptoms for 7 years. The patient attributed his symptoms to TOS. The arrhythmia was triggered while performing an Adson test during the clinical evaluation. … The cardiac plexus receives parasympathetic fibers from the superior and inferior cardiac branches and the recurrent laryngeal nerves that are branches of the vagus nerve. Occasionally, the postganglionic sympathetic fibers may pierce the anterior scalene muscle. Therefore, the authors believe that abnormalities in this muscle may cause sympathetic cardiac hyperactivity. Increased cardiac sympathetic activity appears to be linked with arrhythmias. – Shreeve & La Rose, 2011
Confusion regarding the differentiation between arterial and neurogenic TOS is common because many patients with neurogenic TOS have symptoms of coldness and color changes in their hands along with their other symptoms. These symptoms do not establish a diagnosis of arterial or vascular TOS. They are the result arteriolar vasoconstriction brought on by sympathetic nerve stimulation from compression of the sympathetic nerve fibers that accompany the C7 and C8 nerve roots [2]. – Sanders, 2007
It is clear that the irritation of the cervical sympathetic plexus comes from entrapment of the thoracic outlet. However, the vagus and phrenic nerves have a different course than the above-mentioned, yet are also related to the scalenes. More specifically, the anterior scalene and the clavicular portion of the sternocleidomastoid muscle.
When treating patients with stiff necks, I noticed how some of these had an aggressive cough mechanism occur every time the patient’s head was rotated maximally to one side, usually the side of more significant TOS-related symptoms. It took me a while, but in turn I realized that the vagus nerve as well as the phrenic nerves may get caught between the SCM and anterior scalene, especially when extending or rotating the head. This is often occurring if the patient has a prominent external jugular vein when lying supine, which is indicative of dysfunction.
The treatments are of course the same; the scalenes and SCM requires significant strengthening over a period of time.
Fig. x – 1: m. SCM, 2: m. scalenus anterior, 9: n. vagus, 10: n. phrenicus

Use great caution when treating TOS
Although I am more than confident that my protocol that’s written in this article works, it is important to emphasize that treating TOS is not simple, nor easy. There is a great level of detail that goes into the exercises, as the patient’s body will have learned many compensatory strategies, often for years on end, in order to cope with daily life. The body has especially learned to NOT use the scalenes, as it knows that will lead to a bad time.
Often times the patient will have a difficult time performing the exercises properly. I have spent up to 10 sessions with certain clients until they’ve got it right. That’s not because they are not intelligent, but perhaps had a slight lack of attention to detail, and of course because the body was working against them rather than with them. We have to force the body to re-engage those scalenes.
More so, once the patient does engage the scalenes properly during their homework, their symptoms will exacerbate. This period of exacerbation of symptoms can last all from 2 weeks to 6 months depending on the severity of the situation, and presuming everything is performed correctly (exercises, posture, breathing, etc), and this may of course become a difficult period for the client. It is, however, better than having no treatment at all. And once this period is finished, the muscles can be strengthened without symptoms, and the symptoms themselves will also be gone.
Do not go too hard, too fast
A middle aged woman, dentist and tennis player, came to see me for many issues. Pretty much wide spread pain, much of which was nerve pain stemming from the thoracic outlet. She was having difficulty breathing, clogged ears, neck and shoulder pain, and dizziness. She was also very tired. All symptoms of significant TOS. She was also very, very stressed, worked 10 hour days (with a horrible posture as a dentist), almost without breaks, for 30 years. Of course, time was starting to take its toll.
When she laid supine on the bench, I could see the external jugular vein greatly distending. And even though I hadn’t touched her yet, I knew based on this and the history that this was TOS. I squeezed into the interscalene triangle (into the plexus brachialis) and it caused great pain even with moderate pushing.
I knew that starting to strengthen those scalenes was going to be really rough for her, but because there was so many things going on, we just had to get started. I told her very clearly that her symptoms will surely exacerbate as we start training these muscles; she concurred. We did 5 repetitions the first day, and I texted her the day after and asked how bad her symptoms were. She said that she was fine, and as you know, this implies going a little harder. The next day she did 7 reps, still no symptoms. The day after, she did 10 reps. The next morning, 8 am she calls me; extreme dizziness, can barely stand, a throat so dry that not even water could moist it, difficulty breathing and almost fainting. And of course, big time neck pain. She was stressed out of her mind because patients were waiting for her.
Well, there wasn’t much I could do, as the damage was already done. I told her to take some NSAIDS, which helped some. This is a very unique case and I’ve never experienced something so dramatic before, and I’ve treated many severe TOS sufferers, but that’s also why I bring it up so that you’re aware that this may occur. I don’t know if she trained them (the scalenes) more properly the last day, or if it was the cumulative loading that made the muscles inflammate, but these symptoms are of course vagus nerve irritation as well as vertebrobasilar insufficiency.
She was fine a few days after, but was of course mortified of starting those exercises again. The exercises really aren’t dangerous or scary if adequate intensity is used, but it may take some trial and error to find that “adeuqate intensity”. I’ve already done the trial and error, though, so that you don’t have to. The moral of the story is that if it looks really bad, it probably is, and it may be well worth going easy the first weeks. For this patient 2-3 repetitions PER DAY would be sufficient the first 2 weeks.
Failed TOS surgery, what now?
The most common cause of failed surgery are:
Inadequate resection of the first rib
TOS surgery generally involves resection of the anterior scalene and first rib removal. However, the amount of first rib being removed varies greatly. Dr. Carlos Selmonosky (TOS-syndrome.com) states that they usually moved the shoulder around during surgery to ensure that there was no potential for continued compression after rib resection, either due to the residual stump of the 1st rib, or toward the second rib. This is also noted in the pioneering papers from Roos or Stallworth (done in the 70s and 80s).
The shoulders should be quite uneven in resting posture after surgery, where the operated side will clearly hang much (not a little!) lower than the non-operated side. If the shoulders appear relatively symmetrical in resting height after surgery, this suggests that an inadequate amount of rib was removed. A sagittal plane CT (post-surgery) will help in detecting this.
A large amount of my post-surgical evaluations have symmetrical shoulders and still struggle to lift things or use their arms normally. This is, clearly, because they still compress the brachial plexus toward the residual 1st costal stump. In incidences where the 1st rib was indeed properly resected, the patient is usually compressing the plexus toward their 2nd rib, or have secondary entrapment sites. Read below.
Iatrogenic post-surgical physical therapy
The main point of TOS surgery is to make space between the first rib and the collar bone. Unfortunately, a huge amount of therapists are hurting their patients by cueing them to pull their shoulders “back and down”, or to “relax and drop” their shoulders. Even after surgery, this will either compress the plexus toward the 1st rib stump, or toward the 2nd rib.
The shoulders must be held up in this patient group. They should never be pulled down.
Untreated secondary (peripheral) entrapment sites
Even in incidences of successful surgery, residual entrapment in the periphery may forelie. Evaluation of the axillary nerve under the teres minor, suprascapular nerve under the supraspinatus muscle, musculocutaneous nerve within the coracobrachialis, etc., must be done and treated accordingly. Gentle strengthening once to twice per week of the offending muscle is the appropriate treatment. Worsening of pain means you’re doing too many reps.
Continued bracing / severe psychological distress
Most TOS patients have high stress or anxiety levels and concomitant bracing habits. Bracing worsens TOS tremendously. The patient must be cued to stop bracing, and rest more. If this doesn’t help, anxiolytic treatment may be attempted.
Conclusion
Thoracic outlet syndrome is caused by continuous compression of the nerves and vascular structures. The underlying reasons are often postural and breathing abnormalities that need to be corrected. Secondary to the postural and breathing correctives, it will be important to address all the symptoms; the muscle inhibition. It’s important to work on both the cause and the symptoms in order to resolve thoracic outlet syndrome as swiftly as possible.
Strengthening the muscles that surround the irritated nervous fibers will trigger and worsen the symptoms. This may seem contra intuitive, which is probably why so few are able to manage these types of issues in the first place. However it’s necessary the increase the work capacity of the given muscles to such extent that they no longer irritate the nervous structures that either pass through, or next to them. Some pain in the process is inevitable, so don’t let it scare you. Regulate exercise volume and intensity based on how much it hurts (it should just hurt a little), and start very easy.
Provocative pressure testing is a very reliable way of diagnosing thoracic outlet syndrome, because it shows the therapist exactly where the nerves are irritated. This takes the guess-work away, and the therapist will know where the further assessment and correctives should be initiated in order to resolve the issue.Manual muscle testing of muscles that are responsible for nervous compression, will often reveal a false negative (appear strong) at first. Don’t trust this, as it’s just the body’s protective response. The body knows that firing off that muscle will cause pain and irritation, and often does everything it can to avoid using it.
A quick summary, by points:
- Thoracic outlet syndrome is usually caused by extremely weak scalenes and posturally depressed clavicle
- Underlying causes for the above are often swayback posture, belly-breathing, poor scapular control
- Pressure tests can be performed to identify the exact areas of compression
- The muscles that surround the irritated nerves are almost always weak, and need strengthening
- Strengthening the muscles will make the symptoms worse before it gets better – this is normal and necessary, but shouldn’t be done so intensely that the symptoms become excruciating
References
- Atasoy E. Thoracic outlet compression syndrome. Orthop Clin North Am. 1996;27:265–303
- Povlsen B, Hansson T, Povlsen SD. Treatment for thoracic outlet syndrome. Cochrane Database Syst Rev. 2014 Nov 26;(11):CD007218. doi: 10.1002/14651858.CD007218.pub3. PMID: 25427003.
- REDMAN L, and ROBBS J. Neurogenic thoracic outlet syndrome: Are anatomica anomalies significant?. S. Afr. j. surg. [online]. 2015, vol.53, n.1
- Sanders RJ, Hammond SL, Rao NM. Thoracic outlet syndrome: a review. Neurologist. 2008 Nov;14(6):365-73. doi: 10.1097/NRL.0b013e318176b98d. PMID: 19008742.
- Hooper TL, Denton J, McGalliard MK, Brismée JM, Sizer PS Jr. Thoracic outlet syndrome: a controversial clinical condition. Part 1: anatomy, and clinical examination/diagnosis. J Man Manip Ther. 2010;18(2):74-83. doi:10.1179/106698110X12640740712734
- Köknel Talu G. Thoracic outlet syndrome. Agri. 2005 Apr;17(2):5-9. PMID: 15977087.
- Robey JH, Boyle KL. Bilateral functional thoracic outlet syndrome in a collegiate football player. N Am J Sports Phys Ther. 2009;4(4):170-181.
- Boezaart AP, Haller A, Laduzenski S, Koyyalamudi VB, Ihnatsenka B, Wright T. Neurogenic thoracic outlet syndrome: A case report and review of the literature. Int J Shoulder Surg. 2010 Apr;4(2):27-35. doi: 10.4103/0973-6042.70817. PMID: 21072145; PMCID: PMC2966747.
- Yoo MJ, Seo JB, Kim JP, Lee JH. Surgical treatment of thoracic outlet syndrome secondary to clavicular malunion. Clin Orthop Surg. 2009;1(1):54-57. doi:10.4055/cios.2009.1.1.54
- Ishimaru D. Late Thoracic Outlet Syndrome after Clavicle Fractures in Patients with Multiple Trauma: A Pitfall of Conservative Treatment. January 2012. Open Journal of Orthopedics 02(03):90-93 Follow journal DOI: 10.4236/ojo.2012.23018
- Connolly JF, Dehne R. Nonunion of the clavicle and thoracic outlet syndrome. J Trauma 1989;29:1127–33.
- Schenardi C. Whiplash injury. TOS and double crush syndrome. Forensic medical aspects. Acta Neurochir Suppl. 2005;92:25-7. doi: 10.1007/3-211-27458-8_6. PMID: 15830962.
- Scaer, R. C. (2011). The whiplash syndrome: A model of traumatic stress. Journal of Cognitive Rehabilitation, 18(4), 6-15.
- Korn LE. A Little-Known Symptom of PTSD and Pandemic Anxiety. Psychology today, 2021. Web article. Available from: https://www.psychologytoday.com/us/blog/rhythms-recovery/202102/little-known-symptom-ptsd-and-pandemic-anxiety
- Vanti C, Natalini L, Romeo A, Tosarelli D, Pillastrini P. Conservative treatment of thoracic outlet syndrome. A review of the literature. Eura Medicophys. 2007 Mar;43(1):55-70. Epub 2006 Sep 24. PMID: 16955064.
- Shah JP, Thaker N, Heimur J, Aredo JV, Sikdar S, Gerber L. Myofascial Trigger Points Then and Now: A Historical and Scientific Perspective. PM R. 2015;7(7):746-761. doi:10.1016/j.pmrj.2015.01.024
- Magee D. Orthopedic Physical Assessment 6th Edition. Elsevier publishing, 2014.
- Swift TR, Nichols FT. (1984). The droopy shoulder syndrome. Neurology 34, 212- 215.
- Watson LA, Pizzari T, Balster S. Thoracic outlet syndrome Part 2: Conservative management of thoracic outlet. Manual Therapy 15 (2010) 305e314
- Tolson TD. “EMG” for thoracic outlet syndrome. Hand Clin. 2004 Feb;20(1):37-42, vi. doi: 10.1016/s0749-0712(03)00089-1. PMID: 15005382.
- Passero S, Paradiso C, Giannini F, Cioni R, Burgalassi L, Battistini N. Diagnosis of thoracic outlet syndrome. Relative value of electrophysiological studies. Acta Neurol Scand. 1994;90:179–185
- Veilleux M, Stevens JC, Campbell JK. Somatosensory evoked potentials: lack of value for diagnosis of thoracic outlet syndrome. Muscle Nerve. 1988;11:571–575.
- Aminoff MJ, Olney RK, Parry GJ, Raskin NH. Relative utility of different electrophysiologic techniques in the evaluation of brachial plexopathies. Neurology. 1988;38:546–549.
- Rousseff R, Tzvetanov P, Valkov I. Utility (or futility?) of electrodiagnosis in thoracic outlet syndrome. Electromyogr Clin Neurophysiol. 2005;45(3):131-3.
- Kwee RM, Chhabra A, Wang KC, Marker DR, Carrino JA. Accuracy of MRI in diagnosing peripheral nerve disease: a systematic review of the literature. AJR Am J Roentgenol. 2014;203:1303-09.
- Fishman LM, Dombi GW, Michaelsen C, Ringel S, Rozbruch J, Rosner B, et al. Piriformis syndrome: diagnosis, treatment, and outcome -a 10 year study. Arch Phys Med Rehabil. 2002;83(3):295-301.
- Komanetsky RM, Novak CB, Mackinnon SE, Russo MH, Padberg AM, Louis S. Somatosensory evoked potentials fail to diagnose thoracic outlet syndrome. J Hand Surg Am. 1996;21(4):662-6.
- Sanders RJ, Hammond SL, Rao NM. Diagnosis of thoracic outlet syndrome. J Vasc Surg. 2007 Sep;46(3):601-4. doi: 10.1016/j.jvs.2007.04.050. PMID: 17826254.
- Laulan J, Fouquet B, Rodaix C, Jauffret P, Roquelaure Y, Descatha A. Thoracic outlet syndrome: definition, aetiological factors, diagnosis, management and occupational impact. J Occup Rehabil. 2011;21(3):366-373. doi:10.1007/s10926-010-9278-9
- Selmonosky CA, Byrd R, Blood C, Blanc JS. Useful triad for diagnosing the cause of chest pain. South Med J. 1981;74:974-949.
- Selmonosky CA, Poblete Silva R. The diagnosis of thoracic outlet syndrome. Myths and Facts. Chilean J of Surg. 2008;60(3):255-261.
- Selmonosky CA. The white hand sign. A new single maneuver useful in the diagnosis of thoracic outlet syndrome. Southern Med Journal. 2002;85:557.
- Powers SR Jr, Drislane TM, Nevins S. Intermittent vertebral artery compression; a new syndrome. Surgery. 1961 Feb;49:257-64.
- Kojima N, Tamaki N, Fujita K, Matsumoto S. Vertebral artery occlusion at the narrowed “scalenovertebral angle”: mechanical vertebral occlusion in the distal first portion. Neurosurgery. 1985 May;16(5):672-4. doi: 10.1227/00006123-198505000-00017. PMID: 4000441.
- Dadsetan MR, Skerhut HE. Rotational vertebrobasilar insufficiency secondary to vertebral artery occlusion from fibrous band of the longus coli muscle. Neuroradiology. 1990;32(6):514-5. doi: 10.1007/BF02426468. PMID: 2287384.
- Hardin CA, Poser CM. Rotational Obstruction of the Vertebral Artery Due to Redundancy and Extraluminal Cervical Fascial Bands. Annals of Surgery. July 1963;158(1):133-137
- Alcocer F, David M, Goodman R, Jain SK, David S. A forgotten vascular disease with important clinical implications. Subclavian steal syndrome. Am J Case Rep. 2013;14:58-62. doi:10.12659/AJCR.883808
- Saxton EH, Miller TQ, Collins JD. Migraine complicated by brachial plexopathy as displayed by MRI and MRA: aberrant subclavian artery and cervical ribs. J Natl Med Assoc. 1999 Jun;91(6):333–341.
- Chahwala V, Tashiro J, Li X, Baqai A, Rey J, Robinson HR. Ann Vasc Surg. 2017 Feb;39:285.e5-285.e8. DOI: 10.1016/j.avsg.2016.05.109. Epub 2016 Aug 13. Venous Thoracic Outlet Syndrome as a Cause of Intractable Migraines
- Sell JJ, Rael JR, Orrison WW. Rotational vertebrobasilar insufficiency as a component of thoracic outlet syndrome resulting in transient blindness. Case report. J Neurosurg. 1994;81:617–9
- Larsen K, Galluccio FC, Chand SK. Does thoracic outlet syndrome cause cerebrovascular hyperperfusion? Diagnostic markers for occult craniovascular congestion. Anaesth pain intensive care 2020;24(1)
- Adhiyaman V, Alexander S. Cerebral hyperperfusion syndrome following carotid endarterectomy. QJM. 2007 Apr;100(4):239-44. doi: 10.1093/qjmed/hcm009. Epub 2007 Feb 16. PMID: 17307751.
- Tehindrazanarivelo D, Lutz G, Petitjean C, Bousser MG. Headache following carotid endarterectomy: a prospective study. Cephalalgia 1992. Volume 12:6 p380-382
- Coutts SB, Hill MD, Hu WY. Hyperperfusion syndrome: toward a stricter definition. Neurosurgery. 2003 Nov;53(5):1053-58; discussion 1058-60. doi: 10.1227/01.neu.0000088738.80838.74. PMID: 14580271.
- Sundt TM Jr, Sharbrough FW, Piepgras DG, Kearns TP, Messick JM Jr, O’Fallon WM. Correlation of cerebral blood flow and electroencephalographic changes during carotid endarterectomy: with results of surgery and hemodynamics of cerebral ischemia. Mayo Clin Proc. 1981 Sep;56(9):533-43. PMID: 7266064.
- Aralasmak A, Karaali K, Cevikol C, Uysal H, Senol U. Open Access MR Imaging Findings in Brachial Plexopathy with Thoracic Outlet Syndrome. American Journal of Neuroradiology March 2010, 31 (3) 410-417; DOI: https://doi.org/10.3174/ajnr.A1700
- Urschel HC, Kourlis H. Thoracic outlet syndrome: a 50-year experience at Baylor University Medical Center. Proc (Bayl Univ Med Cent). 2007 Apr;20(2):125-35. doi: 10.1080/08998280.2007.11928267. PMID: 17431445; PMCID: PMC1849872.
- Yamagami T, Handa H, Higashi K, Kaji R. Brachial plexus injury with cough attack: case report. Neurosurgery. 1994 Jun;34(6):1084-6; discussion 1086. doi: 10.1227/00006123-199406000-00023. PMID: 8084397.
- Kaymak B, Ozçakar L, Oğuz AK, Arsava M, Ozdöl C. A novel finding in thoracic outlet syndrome: tachycardia. Joint Bone Spine. 2004 Sep;71(5):430-2. doi: 10.1016/j.jbspin.2003.07.007. PMID: 15474397.
- Godfrey NF, Halter DG, Minna DA, Weiss M, Lorber A. Thoracic outlet syndrome mimicking angina pectoris with elevated creatine phosphokinase values. Chest. 1983 Mar;83(3):461-3. doi: 10.1378/chest.83.3.461. PMID: 6825480.
- Urschel HC, Razzuk MA, Hyland JW, et al. Thoracic Outlet Syndrome Masquerading as Coronary Artery Disease (Pseudoangina). The Annals of Thoracic Surgery Volume 16, Issue 3, September 1973, Pages 239-248
- Xi Y, Cheng J. Dysfunction of the autonomic nervous system in atrial fibrillation. J Thorac Dis. 2015;7(2):193-198. doi:10.3978/j.issn.2072-1439.2015.01.12
- Coumel P. Paroxysmal atrial fibrillation: a disorder of autonomic tone? Eur Heart J. 1994 Apr;15 Suppl A:9-16. doi: 10.1093/eurheartj/15.suppl_a.9. PMID: 8070496.
- Shreeve MW, La Rose JR. Chiropractic care of a patient with thoracic outlet syndrome and arrhythmia. J Chiropr Med. 2011;10(2):130-134. doi:10.1016/j.jcm.2010.09.002

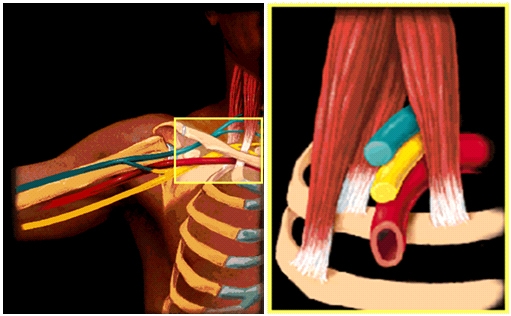








Hi , we spoke about a month ago on my TOS from Canada’s . Just wondering what are you studying on TOS ? Have you heard of this TOSMRI? I did give Dr. Werden your FB link and told him you have amazing case studies. He was intrieged! Keep up the good work . PS I never did get your physio links…….Mona
Dear Mona
I sent you everything on Skype, it is still there in the chatbox.
We are currently studying TOS and its mechanism of cerebrological comorbidities.
Regards
Hi , we spoke about a month ago on my TOS from Canada’s . Just wondering what are you studying on TOS ? Have you heard of this TOSMRI? I did give Dr. Werden your FB link and told him you have amazing case studies. He was intrieged! Keep up the good work . PS I never did get your physio links…….Mona
Dear Mona
I sent you everything on Skype, it is still there in the chatbox.
We are currently studying TOS and its mechanism of cerebrological comorbidities.
Regards
Would a 1st rib adjustment help?
Thanks
No, that’s futile. The scalenes are pulling them up.
Dear Kjetil,
I just want to know what are your thoughts about trigger points deep massages in case of TOS ?
In other words, besides all your recommendations, could trigger points massaging bring something positive to TOS recovery ?
I thank you in advance for your thoughts
Best regards
Tom
Dear Kjetil,
I just want to know what are your thoughts about trigger points deep massages in case of TOS ?
In other words, besides all your recommendations, could trigger points massaging bring something positive to TOS recovery ?
I thank you in advance for your thoughts
Best regards
Tom
Dear Kjetil
Thanks for your helpful artikle about TOS. I want to know more about exercises for strengthening Scalen and SCM muscles. Can you help me? Thank you very much.
See here youtube.com/c/mskneurology
Dear Kjetil
Thanks for your helpful artikle about TOS. I want to know more about exercises for strengthening Scalen and SCM muscles. Can you help me? Thank you very much.
See here youtube.com/c/mskneurology
Ganz toll. Schade das die Videos nicht in deutsch sind. Liebe Grüße
Ganz toll. Schade das die Videos nicht in deutsch sind. Liebe Grüße
Hello,
I Have a 10 year old with EDS, POTS and more. there is a difference of opinion if it’s VTOS or NTOS. Would you be able to give me an opinion based on her ultrasound resukts?
Much Gratitude
Who the hell diagnosed a ten-year-old with all of these diffuse diagnoses?
EDS is genetic with a cascade of comorbidities and POTS is a common comorbidity, why wouldn’t a ten year old be able to be diagnosed with them?
Hello,
I Have a 10 year old with EDS, POTS and more. there is a difference of opinion if it’s VTOS or NTOS. Would you be able to give me an opinion based on her ultrasound resukts?
Much Gratitude
Who the hell diagnosed a ten-year-old with all of these diffuse diagnoses?
Thank you for the helpful information! I know you mention that when you start strengthening the scalenes and other supporting muscles, symptoms could get worse at first. About how long does that worsening last and at what point do you decide that the worsening symptoms indicate that the TOS is getting worse, not better? Thanks!
That depends on many factors. I would need to examine you and take your full history, response to rehab., etc. Generally, review this video:
https://youtu.be/HezNZkdt4Ug
I’ve gotten more information about tos by reading this one article than seeing a bunch of doctors for over a year now.
I’ve got some questions though that I was hoping you might be able to answer/give advice
Thank you for the helpful information! I know you mention that when you start strengthening the scalenes and other supporting muscles, symptoms could get worse at first. About how long does that worsening last and at what point do you decide that the worsening symptoms indicate that the TOS is getting worse, not better? Thanks!
That depends on many factors. I would need to examine you and take your full history, response to rehab., etc. Generally, review this video:
https://youtu.be/HezNZkdt4Ug
This article connected a lot of dots for me and I really appreciate the information. I have TOS and in therapy we have found that my arm becomes very full, fatigued and discolored when I do external rotation. Nothing else really makes it do this. Any thoughts on what may be being compressed here? Is it possible that the external rotators are pressing on a vein or artery? Thanks
Subclavian vein compression
This article connected a lot of dots for me and I really appreciate the information. I have TOS and in therapy we have found that my arm becomes very full, fatigued and discolored when I do external rotation. Nothing else really makes it do this. Any thoughts on what may be being compressed here? Is it possible that the external rotators are pressing on a vein or artery? Thanks
Subclavian vein compression
I wish you were a doctor around here. For me its neck, shoulders, upper arm and fingers mainly index and thumb. I haven’t noticed any bulging vessels or swollen anything but i do have tinnitus and stuffed ears. My doctor has me doing standard PT and it has relived the pain somewhat. but after reading this I’m not sure if its the right thing.
Would a knotted muscle in the neck or suprascrapular area cause symptoms similar to TOS? I went to therapy for TOS, but didn’t seem to help – but worsen my neck it seemed. I found your site and did the head exercise, not letting it reach the floor – seemed to have helped a lot. But problem hasn’t gone away. I was told it may be a knotted muscle in neck, so I am wondering if this could be just a knotted muscle in shoulder neck area.
The scalenus muscle is in the neck. Please read the article before asking questions. “My problem hasn’t gone away”, well, you don’t know what you’re suffering from nor what muscle to treat.
Kjetil, thank you very much for the detailed article. I’ve been working on the scalene exercises with a fairly low number of reps (5) and I’ve been noticing some numbness/tingling on my face (near the chin and side of my cheek), even when resting for three days between sets. Is this something I should be concerned about, or have you seen this before? Should I reduce the exercise intensity?
That’s fine, you’re just doing too many reps or the frequency is too high. Find a rep range / frequency ratio where you get worse only 1 day after training. I usually have my patient train twice per week. See my “reps and sets” video on youtube.
Did the dentist and tennis player recover from TOS after her initial flare from the exercises?
Thank you for this amazing info. I have been doing the scalene exercises 2-3 times per week for a few weeks. It is wild how much weaker my TOS side is. Sometimes I can barely get them to activate for just one rep. I hope you can spread the good word about TOS help to the PTs in America. None of them seem to understand. Thanks again.
She never returned.
TOS exceeds the competence of PT. Seek a PMR doctor with TOS specialty or a cardiothoracic surgeon.
Is pt recommended after surgery ?
No
How could thoracic outlet cause face pain? Medicine student asking, btw
Referred pain through the cervical plexus, or direct irritation of the cervical plexus between the scalene or levator scapula. It will only affect the inferior proximal mandible and ear though.
Hi Kjetil. Do you recommend any specific exercises of those you have made available on Youtube for people suffering mainly with facial and ear pain?
Depends on cause. TMD w. Costen’s syndrome is a common cause of what you’re describing, and you can considering looking into that. I can’t tell you anything specific without consulting with you.
Hello,
I am a 36y old women, born with erb Palsy in the R arm. During the physiotherapy ( treating a low back pain) the professional didn’t pay attention to my pre-existing condition and gave me an exercise that forced alot my good arm ( left arm, cobra in elbows) . After a while I developed pain in my L shoulder with tingling, numbness and swollen arm.
Ultrasound showed tendinitis and bursitis, however after 9 months nothing got better. I have tension all the upper left extremity with neck tightness ( the impression that le carotide is trapped ) . The Dr didn’t want to give me more exams, so I cannot validate the diagnosis , but after reading your explanation it is 99% TOS.
MY QUESTION IS:
DO you know someone that could help me ij Canada ( MONTRÉAL) or what exams to ask for to be able to validate my diagnosis as one of the doctors says it is in my head.
Thank you
Wow this article has brought so much light to something my dr and I have been searching for! I have been having pains in my shoulder for years and just within the past 2 months have been having issues with pins and needles, numbness, Raynaud’s phenomenon, splinter hemorrhages in my fingernails and quite possibly cutaneous micro-emboli’s. All on my left side. I was diagnosed with Essential Thrombocythemia at a very young age and we just assumed it was linked with that disease but now we will be testing for TOS. Thank you so much for the information. Wish you were in the US!
Do you also advise on post-op TOS? Is anything from this information relevant for post-ops?
Fair request, I’ll write some extra material for this topic
You are the man!!! I always loved your YouTube videos. Was very impressed by how much the article made sense and then seen you wrote it! No shock there. Was trying to figure out a connection between dizziness issues and this exact area feeling like it was the culprit. Started reading this and it definitely has something to do with it. Will let my physical therapists know its time to quit massaging the scalenes and make adjustments to my pelvic and low back. Genius
Keep up the good work.
Been dealing with this TOS for years, EMG tests showed no nerve action my serratus. My scap is usually in pain and my shoulder feels numb and whole arm feels heavy and dead. This article has driven me to switch up my gameplan on how to heal this.. i guess im going to have to follow the pain and work these dead muscles up again and hope that will regenerate nerves and pull the bone off them.. thanx for help brother
EMG and neurographies as such are useless in the diagnosis of TOS.
Hi kjetil. I believe I got TOS after a rotator cuff tear/possible brachial plexus injury.
Is there a difference in treatment if it was brought about by an injury or if it was just developed over time? Can you please email me. I’d also be interested in possibly skyping with you. Thanks
My apologies, I don’t have the capacity for free back and forths on email. You’ll have to book a session.
This is a great article and explains a lot. Thank you! You mentioned that 10 reps for 1-2 sets once per day is usually a safe start for the scalene exercises. Is this 10 reps for each of the middle and anterior scalene exercises, or 10 reps total (eg 5 each). More importantly, if this is a good start, what should be the max reps and sets I do in a day (ie the point at which I won’t really be getting any more benefit from doing more reps/sets?)? Thank you again for a great explanation of all of this.
Thanks for noticing this, I’ve edited that. Please see this video.
Reps & sets:
https://youtu.be/HezNZkdt4Ug
Hi,
My scalene I believe the middle one sticks out and is hard to the touch does they mean it’s weak and hypertrophied? Would the strengthening of scm and scalene make this go away? Also I never knew what the neck hinge was called but I asked my doctor about it and he said it looked normal which I knew it didn’t cuz just felt like it folded rather than extended. Also I broke my neck about 6 years ago so I’m sure that’s where the problem is from as well as bad posture. Thank you!
Breaking your neck certainly didn’t make your neck muscles stronger. So, yes.
can i also introduce mobility exercises? I am actually mobilizing my neck and after the mobility I feel a clear irritation of the scalenes and in the area of the clavicle.
Sorry, this question is too vague
Hi, can uneven hips cause this? I have a hypertrophied Scalene on my left side and an elevated hip on my right. I get tingling sometimes and weakness
Not unless you’re as crooked as Quasimodo (ie., extremely crooked). So, not really. It’s generally caused by neck trauma or stress, combined with poor neck and shoulder postures.
We need a comprehensive diagnosis and treatment centre like yours in Canada. We get treated like lab rats being sent from one 15 minute appointment to the next. No comprehensive evaluation, no comprehensive treatment, lots of botox only solutions, practitioner ego and blaming the patient. It is ridiculous what has happened to our healthcare system.
This is why public health care is good if you have a simple medical problem but a tragedy if there’s any complexity to the matter.
When strengthening the upper traps, can this worsen nerve pain? Shrugs have helped but my pain is back. May be overworking…. Thanks
Yes, if you go too low it will compress the plexus. Watch my video on how to do it properly.
Trapezius
https://www.youtube.com/watch?v=dCI-Qa6Fu-Y
I want to do your Scalenus anterior & medius exercises, but can not lie on my side, because I have Ehlers Danlos Syndrome, and my shoulders sublux/dislocate in that position. Is there another way I could do this exercise? Would it be equally effective if I hang my lower arm over the end of a bed, for example? Thanks in advance!
I don’t know. Try.
Hi, thanks for your extensive review. I would like to make you a few questions.
1) Could myofascial scalene release be done plus scalene strengthening for Thoracic Outlet Syndrome to get positive results and get less symptoms in the process?
2) I wasnt surely clear about this after reading the article: Could Scapular problems (scapular dyskinesis) be the cause of TOS with neck and head symptoms?
Thanks
Did you even read the article?
Big thanks for this article and all the videos. I may have to book a Skype call with you. I have several suggestive symptoms for TOS and one is I can’t brush my children’s teeth in the evenings because the trapezius muscle gets tired quickly on the symptomatic side. Is this symptom of TOS?
You’re just weak
🤣
Recently diagnosed with VTOS and suspected NTOs as well but wont know until get in and check the area for fibrosis and nerve entrapment. Seeing horror stories on surgery had me concerned but this article helps me realise what i had been suggesting for years with my POTS and autonomic dysfunction and syncope blackouts seemed related. They always downplayed it but now with VTOS diagnosis i am hoping surgery will resolve this and i can finally get my life back. Am worried ofcourse surgery could make things worse but after no luck for 10yrs and worsening i will be going the surgery route. I thankyou for your article and writing about the connection with venous TOS NTOS and autonmic issues.
Hi man, great article. I have some questions about the scalenes though. How do you differentiate tight scalenes with hypertrophied scalenes? And what would be the exercises if someone has TOS because of the latter? Thanks in advance!
The hypertrophied scalenes you are talking about, are fatty-atrophied. The hypertrophy isn’t real muscle tissue. Thus, if this differentiation was necessary, it would have been mentioned in the article.
Thanks for your answer Kjetil. So the thickness and hardness in the scalenes is because of fatty tissue, correct? And is there a chance the scalenes could be fatty-atrophied and the SCM could be weak and soft?
This article and your scapular dyskinesis article have helped me immensely. Previously had pain for 1.5 years. Since I started exercises and posture correction changes listed in these 2 articles 1 month ago, I have absent or barely any pain if I keep my L shoulder up but it definitely still has to be conscious act. My question is regarding my tight lats contributing to my symptoms that feel relief upon stretching. Based on your statements of a tight muscle being a weak muscle, is it a good idea to incorporate exercises such as lat pull downs or pull ups in an effort to give relief to my tight lats?
If your lat was so tight that it altered your scapular mechanics, you wouldn’t be able to lift your arm.
Rather, this is probably just some kind of bracing issue and you’re using the wrong muscles. I recommend working on scapular motor skills and disregarding other things like as strengthening until you’ve got the basic movements down
Hi Kjetil. What are your general thoughts on having a rib-sparing scalenectomy, especially in TOS-CVH? Does the more conservative procedure make sense in some situations?
My CVH symptoms are greatly exacerbated by doing even one rep of the scalene exercise, but I have little pain and few problems lifting weights or using my arms normally, at least when I don’t raise them overhead. So I was thinking that I might not need my first rib removed.
Then I would consider surgery. Surgeons have told me mixed things about scalenectomy-only surgery; one of the main things is the risk for reattachment to the rib after snipping it. I think I would probably opt for resection of the rib and 1st scalene if I were you.
with due respect Larsen, I could assign the jawbones position hundred percent for the reason of such problems, backward maxilla and mandible cause scalene drop and so on … . never gonna happen when both jaw fully grown upward and forward.
What absolute garbage.
Dr James Stoxen says in his book
that we have to eliminate all the inflammations and triggerpoints in the 10 muscles that compress the tos, before we Beginn to strenght.
[The total treatment time for this patient could be 29–30 hours with no breaks on a severe thoracic outlet syndrome case. Now remember, these patients have been to many different healers, they have had thoracic outlet syndrome for 2–10 years, which means the reflexes are locked deeply in the brain and there might be a lot of scar tissue in the muscles and joints.]
These are the 10 muscles that compress the tos
1. Anterior scalene muscle 2. Middle scalene muscle 3. Posterior scalene muscle
4. Anterior cervical (neck) muscles 5. Subclavius muscle 6. Biceps short head muscle 7. Coracobrachialis muscle 8. Pectoralis minor muscle 9. Latissimus dorsi muscle 10. Lower trapezius muscle
So im very confused because you say that myofascial Release is not necessary.
Good luck with that
What about sinuses problems from TOS? When I do the exercises, not only I feel that my mouth dry up but also my sinus, making breathing trough the nose very hard. When I exercise I basically know the following night my nose is going to bother when going to sleep. Feeling so thirsty that no water can saciate me is one of the symptoms I started to develop as a pre adolescent when breathing became a problem. It makes sense tough, cause my nose is pretty much always clogged up. Thats what I think this mewing trend is missing. Mouth breathing is a posture problem that the Mews only know in a more superficial way compared to you. After reading some of your material I believe rhinitis, hard time breathing trough the nose and also sinuses problems might be muscle skeletal and neurological related. My nerves can also get irritated when I jaw jut, causing either pain in parts of myhead/face/behind the ear and feeling like there is something stuck in my throat causing sickness. I see some of the Mews instructions are absolutely detrimental after reading your stuff. Holding teeth together, chin tucking or simply saying that people breath trough mouth due to laziness is non sense. You are the man who made it, you solved the puzzle. Thank you and congratulations! I have been following the protocol for a couple of months and even tough things go slow, I am definitly seeing a change…
Doubtful
Hello Kjetil, I have a background on pilates & they say you have to activate TVA & pelvic floor to change your posture. Is that even necessary? Thank you!
Yeah what do you think about this Kjetil? It’s an interesting question. To further expand on Juan’s question, is activating the TVA and stabilizing the pelvis the only way we would be able to hold the position of keeping the scapula raised in a slightly upward testing position?
Swayback posture is a common cause of excessive anterior tilting and dyskiensis of the scapula. That said, this develops over years and years. I recommend working on thoracic posture and angles (swayback) as an underlying cause when treating dyskinesia, but not as a direct intervention. You can keep your scapula up in the proper position, if conscious of it, regardless of your pelvic or TVA status
Pilates teachers say a lot of inaccurate things that will get you hurt.
Now to answer your question, no, it is not necessary.
I do generally recommend TVA activation in posture (gently sucking the lower abdomen “in”), but I have not found any activation necessary unless the patient has obvious problems with either urinary or fecal incontinence that occurs, eg., with impacts. Rather, clenching of the PF can cause painful syndromes, especially coital pain.
Hello Kjetil
When I round my shoulder my collarbone clicks and just wanted to know me doing the shoulders up posture will help this. also wanted to know if dead hanging is doing it any damage as I have started doing this.
Hej Kjetil,
A few questions.
I understand that ultrasound is one of the standard examination.
Do you know if it can be difficult to see a vascular TOS with ultrasound, even be false negative?
Do you possibly know if there is a TOS specialist in Sweden, or where the nearest is?
Thank you very much for your educational and specific information.
/Anna
Very very high false negative rate
Amazing write up. So informative. I thought my TOS might have been just genetics or purely innate anatomical defect in nature.. But I also have atrocious posture and have for years (gotten especially worse over pandemic and working from home so much). I’ve been suspicious of my posture causing my problems. I’m still quite active (weight lifting, drumming, yoga). I decided to try to fix this on my own (shoulders back and down) and as such I developed an upper extremity DVT (effort thrombosis) of the subclavian vein recently. I have to assume this is from what you said, that it further compresses the thoracic outlet.
My vascular surgeon is recommending first rib resection. But it also seems like I could alleviate a lot of my symptoms from the exercises outlined above based on what I was reading.
I’d love to know; is there a point where PT and exercises won’t help as the syndrome has progressed too far? I’m worried that I’m rushing into rib resection surgery when there may be a more conservative approach first through what you outlined: physio, posture fixing, scalene exercises, correcting breathing, etc. But that being said, it’s been bad enough that I already developed an occlusive blood clot in my subclavian vein and I definitely have neurogenic symptoms. My surgery is scheduled for June 20th.
I would love to know your thoughts.
For something this specific you’d have to book a session
My coracoclavicular ligament was severed in my right shoulder and I had to have surgery. I am sorry to say that I have been left with a deformed collarbone. Ever since the surgery I have had a red swollen arm, dilated veins that make my arm and hand feel like they are going to explode. Plus many dysautonomic symptoms I did not have before. Unfortunately, none of the physicians can explain my “strange” symptoms. I live in South Africa and wish that our doctors had more knowledge on this syndrome.
Amazing article, and so informative. I recently developed a subclavian vein DVT, and found out from there that I have venous and neurogenic TOS. My posture has always been quite bad. Interestingly after spending a few months trying really hard to improve my posture – is when the blood clot formed. Reading your article really shed light on that as I assume it’s because I was doing a lot of “back and down” motions trying to fix it, which compresses the thoracic outlet even more.
I have a first rib resection surgery booked for two weeks from now. But now I’m curious if I shouldn’t try to do these exercises, both scalene and breathing, and fix my posture as per your guidelines before opting for the surgery.
In cases where the SCV has occluded and clotted like in my case. Would you push for first rib resection for release, or attempt these exercises first? I’m really on the fence for what to do. I just feel weird about removing a part of my body without trying something more conservative first.
Surgery and anticoagulation therapy!! You will, however, require help for scapular dyskinesis afterwards. Contact me then.
Have you seen positional purple hand arm with Thoracic outlet syndrome without blood clot? I was diagnosed with nTOS and vTOS a year ago but now I have purplish hand and sometimes swelling in my TOS arm when its by my side, which I didnt have before.
Had a Ultrasound doppler which didnt show problems. Cant understand this symptom, have you seen patients with this symptoms and get a good to go to start your program?
Of course, that is typical VTOS.
Thank you for this comprehensive article. I dare to say it’s one of the few ones that don’t insist on obssesive stretching before there is even a muscle mass to begin just overstreched tissue that wasn t really able to do that in the first place.
3 questions I have:
1. have you succesfully treated arterial TOS with the scalene streghtening thus allowing the return to sports and intentional and performative rotations / tilts of the head?
That is, the resolution of dizzyness when rotsting and tilting the head away of the compressed part.
2. Are there any possible ligaments implications that mighr further compress the structures.
3. What about dancers, and high mobility performers? What if they somehow get this kind of scalene weakness or injury, let s say, from inappropriate return to activity after a long pause. Are they doomed or recoverable?
Thank you!
Hi,
There are a lot of 5-minute-experts out there that insist on a lot of things, interetingly without any genuine results with patients. Thanks.
1. Yes, but remember that the scalene is just one part of ATOS. You also need to deal with the subpectoral and costoclavicular spaces.
2. No
3. Recoverable with the right protocol
What if neck pain is totally gone after resolving scapula position but weakness in grip strength still remain? Would strenghtening the forearm muscles be beneficial in that case?
Either your shoulders are still too low, dyskinesia still present, or you need to be more patient. Probably a combination of all three.
hi Kjetil, thank you for this how to guide. i had a posterior dislocation of my sternocavicular joint and my hypertonic scm seems to be more of an issue than my scalenes. i am seeing a cardiothoracic surgeon in two weeks. i understand one of the first things they will do is botox as a partly diagnostic measure. do you think this is contraindicated where i still have such instability at my scj? i appear to be having arteial tos symptoms, just had one of my worse cold and white hand episodes. thank you for your time. i just want my arm back.
Your SCM would not affect your arm, only – to some extent – the subclavian vein. I think you are misleading yourself by presuming that the pain location is also exactly where it is originating from. The SCJ dislocation is a separate issue.
Botox (scalenus, whiplash, etc) is generally not a good idea unless one is already awaiting surgery.
of course the scm is going to effect the function of the arm! it is the only attachment between the axial skeleton and the arm, if there is movemnet dysfuction at the scm, of course that would play out in arm function!
neck ct shows, “mild narrowing of the subclavian arteries and the interscalene triangles.” all of the symptoms started the day of the scm dislocation and with my hand blowing up!
i have the botox scheduled for in a few weeks. he did not mention surgery. why is botox generally not a good idea unless awaiting surgery?
it seems to be their protocol. always botox first and see the response.
Hello ! This is my files of diagnostics in the format dicom and jpeg (MRI verbal spine neck and MRA agiography
without contrast , MSKT agiography with contrast)) URL https://drive.google.com/drive/folders/180G0B9Ev6UWbGuFIdXjjcgFiqFmJggud . On MRI verbal spine neck where i see wide (big) anterior scalene muscles and vertebral artery located nearby at a distance of 1-1.5 mm. And on this MRI images i saw kimmerly ring (Ponticulus posticus),but my doctors didn’t see it, later they did a multislice computed tomography and then confirmed it)))) Ultrasonic diagnostic and Adson test diagnosis is negative for scalenus syndrome, but found compression of the vertebral arteries when turning the head, at 1 cm at the level of the C2 vertebra (atlant) from 45 cm/s up to 125 cm/s and on right up to 82 cm/s. the doctors again excelled, they saw compression only on the third attempt))))) Well, after that I myself saw the kimmerly rings on the MRI images.so I suppose that maybe there is still a little scalenus syndrome. Willis circle ?Maybe a plexus of veins ?(it is unlikely that the jugular vein) Symptoms: whistling (ringing) in the head, sometimes stuffs up the ears, after lifting weights, the whistling (ringing) intensifies – nasal congestion, there is a lack of air, a cloudy spot in the eyes, fatigue, I never get enough sleep in the morning and a mesh in my eyes. At night, lying on your back, you wake up with a slight dizziness, which passes quickly. in 2012, I slept on my stomach for 3 hours a day for a month, one hand under my forehead and the fingers of the other hand under my mouth, for breathing. for a week I felt like a different person, I was cheerful energy and strong, there was no whistling (ringing), my nose was breathing. I stopped sleeping on my stomach and everything came back.
I had tos surgery jan 3rd 2022 right 1st rib removed 3 hypertrophied scalene muscles and subclavian artery dissection with pec minor release got better for 1 month after the surgery did 7 months of pt following the surgery and 18 months of pt prior to surgery, now I’m constantly tachycardic 120-170 bpm especially when turning neck or using arms, mottling on my legs, hand and feet, nausea, severe headaches neck tightness, heavy head and electric shock like head, ear pain, pupils different sizes, chronic tinnitus, rapid weight loss Gi issues, sweating alot for no reason only sweat on one side of my head, black out, dizziness, severe brain fog, pain all over my body and no one can figure out how or why my Autonomic nervous system is going haywire, had a new emg done I have chronic reoccurring brachial plexopathy and now a arterial component on my left arm loose pulse hands change colors arms constantly hurt, Vascular surgeon will not do any further test or order any vascular studies as I had surgery and should be “FIXED”
PT probably made you worse. I don’t recommend PT after surgery, as most PTs have no clue how to treat this problem. Surgeons should be aware that any PT that cues their patients to depress their claviculae will WORSEN the patient’s symptoms and screw up the surgical results. I strongly suggest that you book a consult.
Can these TOS exercises cause POTS symptoms? Sweating more often (when I first get up in the morning)?
Yes, because it raises head arterial pressure (and this lowers body pressure)
But can this exercise improve POTS due to thoracic outlet syndrome?
Hey Kjetil,
I am in the process of trying to figure out if I have vascular TOS. When I press on my left scalenes, I can induce nystagmus. The muscle feels tender from my collar bone all the way up to my ear. When trying to hold my shoulders up (as you recommended in your TOS video) I notices a fatty bump right where my collar bone is. Is this a sign of fatty-atrophy?
I also, just found out that I have elongated styloids on both sides. I am in the middle of trying to figure out what is causing my symptoms. I have been trying to follow some of your programs and it seems to be affecting my vagus nerve and causing a lot of anxiety. Is there any way to know if this is a styloid problem, or scalenes/SCM?
Would need to review your case and imaging. If you’re trying to figure this out on your own with no clinical or imaging experience, I think you’ll end up regretting it.
Thanks for the reply. I will be booking an appointment with you soon. I have MRIs (head, neck), 3D CT, and CTA. Will that be good for a first appointment?
Also, can TOS cause an elevated heart rate with palpitations without cervical rotations?
Thanks for this great article.
Regarding the exercises part, If it’s hard for the patient to start right away working on these muscles, would swimming 2/3 times a week be an alternative to strengthen the neck, shoulders and back? You know, because of the less-resistance nature.
Hello Kjetil
I am pretty happy experiencing symptom improvement when following your advice/protocols strictly(for TOS).
1)Should I do some neurovascular workups while i am rehabbing and get back to you through Skype after completing them ? For evaluating the compression site(s) of TOS for instance.
2)I am already doing your regular SCM-exercise, is there any worth to doing your other SCM-exercise for the clavicular head(I tried it one time, and it gave me a bit of worsening headache/pressure right after so I shied away from it)?
I understand if you rather want to answer these question through a Skype meet.
Hello Kjetil
Thank you for all the information you provide firstly. I had my Tos surgery 20th august 2022. I was diagnosed by ATOS after ct angiography. Pre surgery i had some range of motion issues on my related side tight scm, scalene muscles and trap pain. No significant loss of power with my arm but this back pain was not allowing to use arm comfortably upwards above certain angles.
Operation includes 1st rib resection, scalanetomy with subclavicular approach. 6 days post surgery i had terrible pain all over the place with shortage of breath and it came out to be hematoma. Needed a resurgery to clean that up.
Meanwhile i was having some complaints about my other side with different kind of symptoms which were 4th 5th finger weakness loss of grip power, wrist ache etc.
Another doctor diognosed Ntos on that side and 40 days after first surgery i went trough another one.
Result of this one was post op horners syndrome and lower trunk damage. Ulnar nerve damaged significant loss in grip power and lots of neuropathic pain for almost 2 months. While suffering from these i had no complaints about my first operation side my back was okay i only had pain at incision and some sort of pain when i raise my arm but it was not a big deal.
Used Lyrica 300 mg for a month for my neuropathy. I gradually ended using it with docs advise got better and better with my symptoms however by the time i am getting better my first operation side back pain symptoms neck stiffness shoulder blade pain started to aggravate. (4 months after surgery). I started psychotherapy, no exercises just massage ultrasound therapy, neck traction, and heat therapy. Sadly it only kept going worse over time.
Its been 5 months after first surgery now i had the worst scapular pain ever my neck is so stiff and i have lots of muscle knots around my scapula. I got back to work but these symptoms making my life harder than ever. Doctors think my operation was succesfull the advised to start exercises even tho it makes the symptoms worse for a while should keep doing it for some results. They also start saying that this is fibromyalgia. I am so confused and don’t know what to do. Sorry to keeping it too long, your advises will be soo much valuable for me. P.s before this disease i used to be an athletic guy with strong back muscles.
Thank you for your time
Great article, amazing work. Thank you.
In your general opinion, do you think subclavian vein compression upon abduction should be surgically decompressed even in the absence of a clot? Or would you pursue “conservative” approaches first, so long as no clotting is involved? I’ve gotten 4 different opinions from vascular surgeons. I am just curious on your general opinion on conservative approaches to vein compression in TOS, or if you think any compression means surgery is required. Thank you!
Your question here suggests that you have not read the article.
Positional impingement of the neurovascular bundle happens for two reasons. 1., and mainly, because the collar bone is too low during articulation of the arm. 2., because the pectoralis minor is too tight. Neither requiring surgery if a correct treatment protocol is utilized.
Hi Kjetil, amazing articles – on TOS, Winged Scapula, subluxing clavicles and TMJ/D. I suffer all of these things. I have had two mild concussions hitting the forehead (one at 13, one at 28) and I have an underbite. I have had neck pain since my teen years, and now at 32 it has gotten unbearable and general UK physio is not fit for a complex case. I believe I have TOS/Winged Scaps which is causing a lot of this – when I pull the funny face on the cover of your Muscle Clenching article I get some numbness in the SCM on the side where I have the suspected TOS – is this a sign?
Do you think there is non-surgical hope for me (I have EDS and POTS too) or is this going to be something that will need the right specialist to truly resolve?
Many thanks – your articles have taught me more than any NHS nurse or doctor or physio i have seen in my 32 years so far.
Do not know on which post to ask so I ask here. I’m pretty sure that I don’t have TOS. I have good scapular positioning and none of the test are positive for me but my upper back is really painful on t5/t6 level on right side. It shows when sitting for longer duration (like > 45 min) paraspinals at that level are getting very tight(muscle spasm?) and pain radiates below scapula/lateral side of the trunk. Tried cervico-throacic extensions as an exercise but it doesn’t seem to work, I suspect that can be facet joint arthritis (but im young male) or intercostal neuralgia? Do you have any thoughts on my case? Thanks!
Either you’re doing the tests wrong (most likely), or it is a spine problem. If you’re having upper back symptoms and intercostal pain that worsens with arm-loading then it is almost definitely TOS.
My pain doesn’t come with arm loading. I even forced to have my right scapula at very high level for a couple of days cause I thought that I can have my first rib higher and still crush brachial plexus but it didn’t helped. Do you think that is possible that I have thoracic hypermobility, it is even a thing? Do you think that conservative treatment can help? Thanks.
I would have to review your case to give an opinion; I can’t say just out of the blue. A couple of days though, yeah, that’s often not enough.
I have read a lot of your facebook/instagram posts and one of them catched my attention. Its from December 2017 about stuck facet thoracic joints and unilateral weakness of longissimus cervicis affect on them. Tried stretching like you said there and it helped. You recommended then doing cervicothoracic extension simultaneously with slight ipsilateral cervical rotation. Tried it but it dosen’t seem to target that muscle for me (i was lying down from bed). After these years did you have come with a new exercise or tips for this condition?
Dear Kjetil,
thank you so much for your efforts in this field. I have visited more than 70 doctors in 10 years and no one was able to diagnose my condition until I showed your articles to some of the local doctors and they did some of the tests.
Finally they concluded that I had TOS and prescribed PT for 6 months, but it really did not work because they had no idea what they were doing (they were trying to stretch my neck muscles, etc which made everything horribly worse). In the end they did a surgery, as I was completely losing pulse when I turned my head on one side. Surgery helped little bit, but I would say that 60% of my symptoms still remain (I cant drive with right hand, even when I brush my teeth I get weakness, I am often dizzy, have intermittent visual problems, I feel extreme tension under my jaw, right sight of jawline and in neck, I lost ability to play fast passages on guitar or piano, etc).
I am determined to treat this condition, I have watched every one of your videos and read your articles, but it is very difficult to self-navigate the whole process, there are so many muscles involved and every little detail matters. Self-evaluation is very hard as well when you don’t have relevant knowledge. Unfortunately, I don’t have resources to pay for sessions for months and I was hoping to get some suggestions from you, is it possible for someone to do the rehab independently, without having all your knowledge? Moreover, can you please make playlist on YouTube of TOS relevant exercises?
I cant take this torture anymore, it has worsened every aspect of my life for more than 10 years. Thank you again very much, I think you are the only one out there who can help people like me!
What are your thoughts on fibrous replacement of the subclavius muscle in regards to tos.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8742971/
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9256487/
https://www.pulsus.com/scholarly-articles/bilateral-fibrous-replacement-of-subclavius-muscle-in-relation-to-nerve-and-artery-compression-of-the-upper-limb.html
My pain started more as a “heating up” of the pronator teres (forearm?) about 5 years ago. You can put an infrared thermometer at my arm, 102+ and anywhere else on my body will be a normal (for me) 97.8. Eventually it began to ache more. Then, five months ago, the pain extended to my upper arm, and under the arm. I cannot carry even my purse. I have lupus. I thought it was just another flare that would eventually go away but 5 years later, not only did it not go away, it got worse. The pain shoots up to my collarbone if I forget and lift my arm too high and even worse if I accidentally carry something. Do you think this is possibly something I should look into as a reason with the specialists you listed above? I already see so many doctors for the lupus. Rheumatoid, Heart, gastrologist, nephrologist, urologist, psychiatrist, neurologist, endocrinologist, dermatologist. I have no idea which one to talk to about it. I mentioned the heat/temp thing and I think my rheumatologist thought I was nuts. I brought it up to my dermatologist (I am UV sensitive) because I thought maybe it was a photosensitivity issue, she had no clue either. It’s hard to prove because it comes and goes. Who would make up something that ridiculous.
Hey Buddie,
this is my result of an nerve sonographie. What do you think i should do exactly? I am scared of a surgery. Is there a conservative way for me?
Nerve ultrasonography: Supraclavicular cervical roots C5-C8 were unremarkable. Hypertrophy of the scalenus anterior muscle on the left side was suspected. As an anatomical variant, the roots C5 and C6 on the left side do not run in the hiatus gap but in the scalenus anterior muscle. Infraclavicularly, a prestenotic signal with decrease of flow below 100 cm/s can be detected intermittently on the left side at 90° abduction, in addition pectoral stenosis with Vmax around 200 cm/s. On the right side, stenosis in the subclavian artery with Vmax above 200 cm/s can be detected only during the special maneuver described by the patient with retraction of the scapulae and lowering of the clavicle. Venous stasis cannot be detected on both sides.
Thanks in advance.
Only means positive for TOS. The clinical symptoms would determine severity, not this test.
I have been diagnosed with TOS after years of migraines & other signs. Reading this makes me feel not so alone & explains a lot of the hell I have been through. Thank you so much. I also several years ago fell backwards off a porch & jammed at least 4 vertabre & it is on my brainstem. I was told by a seated neurologist to go home and take my medicine which I am OCD about. I write down each time I take it. It just helps to know that I am not alone although I would not wish this on anyone. It also switched my days & nights. I sleep now in the day & stay up at night. It does not go over with most people. They do not believe me.
I suggested TOS 5yrs back. The nerve conducting test performed laying on my back showed nothing. My symptoms started around 30, after my breast reduction, H to C+. Forearm knots just below elbows and Ulna nerve leaving track mid 30s. Mid 40s there were two vehicle wrecks and a hard full body fall.
After that I developed so much pain I couldn’t keep up. Started going to Dr’s who couldn’t see past my Polyostotic Fibrous Displasia, called it anxiety.
When the pain got so bad, I could no longer handle Anything around my ribs or weight on shoulders. I have given up any attempt at a bra.
I was diagnosed hypermoble in ’21 and now my 30 yr old son is headed for disability with shoulder and knee refusing to stay in socket, spine slipping. Seeing a geneticist for hEDS eval.
I have horrid bone lesions in ribs, spine, skull, collar bone, etc. So I’m game for strengthening but may not get far.
Currently having disautotomia, unable to lift anything, pain in back, shoulders and neck, vagus nerve flares(like panic attacks), numb thumbs, nervy skin on arms.
Taping from c7 spilt front and back of shoulder both sides creates tremendous relief and freedom of movement.
Do you belive that in EDS cases, where heavy breasts can’t be supported, that removing the breast weight would relieve the entrapment?
The breast is just the tip of the iceberg. I’ve seen so many patients get implants, “get TOS” (reality, just last drop) -> take the implants out, and NOT recover. The breast implants aren’t causing this; the low clavicular height is. Now, are hypermobile patients more susceptible to get TOS? In my experience, yes.
What could cause random lateral/posterior delt “nervy pain” that lasts for a little while and resolves on its own even when shoulders are definitely held “up”?
Quadrangular space irritation, for example.
hi Kjetil, the long term impact of a scj that is unstable do to a trauma involving a posterior dislocation. what happens to the rest of the upper extremeity after 4 years of scj instability? a dislocated ac joint, an inferior dislocation of humeral head, distal humeral head sublexed and tore ucl, then distal ulna sublexed, tearing then druj instability. occipital and spenoid involvement issues, causing major eustuchian tube issue. the head is in such poor aligment that even internal pressures are effected! when try to move neck, the eustuchian tubes can be felt trying to move back into place. an arm that can no longer function in life, bc no one understand the consequences of an extremely unstable sjc, that was caused by a high speed trauma, where the scj was dislocated!
I think whiplash is a more possible problem here than the notion of a bad SCJ leading to the myriad of problems you have developed
and you are right until not doing boto until you are awaiting surgery. anterior and medial scalene botox can lead to major eustuchian tube issues!!!!!!!!!!!!!!!!!!!!!!!1 you heard it hear first! the tos doctor denies that cervicogenic diziness can be brought on by botox. i don’t get their not knowing how the body connects.
What are your thoughts on the Edgelow method for TOS?
Don’t care
Can sore lower right ribs and sore right hip be connected to TOS? I suspect I have TOS on this side as well. May need to book a consultation
I have recently been diagnosed with ATOS. A year ago I had passed out getting out of bed, and landed with my left side up against the wall. What originally started with my left shoulder feeling off, has led to over a year of regular PT appointments, 3 doctor appts, multiple x-rays, regular chiropractor appointments, ultrasound, neurologist, spine specialist, and several MRI’s. The last MRI was of the brachial plexus, which finally showed the compression of the subclavian artery. Like many others, the symptoms are life impacting.. and you begin feeling like nobody knows what they’re doing. It is amazing how quick specialists want to do surgery. At this time, I am hoping to avoid surgery due to the mixed reviews I read. I do have the poor posture, with forward shoulders, and do believe the clavicle is a culprit. As well as, my thoracic and hips seem to be off, even with regular chiropractor adjustments. Currently my PT is working on the Pec Minor, Lats, SCM, and scalenes, as well as traps and deltoid. I found your article very informative and was hoping to find a more structured outline for treatment to share with my PT, as well as for myself to do at home. Any help would be greatly appreciated, as again, I am hoping surgery will be a last resort. Thank you!!
Hi Kjetil,
Thank you for publishing this, though I wish it was the first article I had read rather than 4 days after onset of my problem; it is by far the most comprehensive article I’ve read out of hundreds.
I believe I have TOS and getting a diagnosis and treatment has been difficult. I have now sat with 3 doctors who have done the same google reading as myself, and who have recommended as treatment that which you have said should be avoided (namely stretching the scalene muscles, the pec minor, infraspinatus and subscapularis). I have stopped as I feel it made it worse, and I’m following what you have written, since thus far you have most accurately described my experience. Especially the lowered shoulder and pec major, which no doctor I have seen has yet commented on. I plan to share this with them.
Posture is a problem for me, particularly in my pelvis and shoulders, and I’m also a high-level swimmer though I have greatly reduced my training regimen. I believe this started years ago with nTOS and has since progressed to vTOS after I injured my infraspinatus or subscapularis while swimming recently. Possibly from compensating for the injury? I’m not sure, but would not doubt it.
If I could ask you a few questions about TOS:
1. Do you often observe severe swelling around the clavicle and over the pec minor in TOS? My clavicle is no longer visible on my right side (no blood clots observed as of yet). I also experience spasming in my pec minor and major.
2. I’ve also noticed that slinging my right arm across my chest and grabbing my left pec/shoulder seems to help the blood drain (veins in my arm stop bulging, and feel similar though slightly harder than my good arm), but given this is often a postural problem are there any concerns with doing so?
3. Lastly, would you recommend ice or heat as treatment? I am allergic to NSAIDs and Tylenol does nothing for the pain. One of the above-mentioned doctors has prescribed baclofen, which I believe is also doing nothing.
Thank you in advance for your time,
Erik
What is really the cause of that lowered scapulae/shoulders in TOS people (and really others not symptomatic)? Do the breathing pattern plays a role here eg. not expanding upper chest? For me it looks that whole form collapses downward: the mandible opens, scapula lowers etc. Do you have some idea?
Stress, low self esteem, lack of proper postural guidance / role models during upbringing
Thank you for sharing incredible knowledge in this area. Like so many commenting, I have had no answers and massive gaslighting on my suspected TOS for decades creating a feedback loop of stress and anxiety in the body. Broken clavicle in my teens and cervical plexus involvement with chronic cough, scalenes that are weak/tight on one side and longstanding issues with the inferior mandible on that same side plus odd compensatory swallowing patterns that then put the whole upper mandible out laterally as well. The TOS aspect to my case is roundly ignored but in my search for answers I have recently been told my tongue-tie (around 30% tied) that I didn’t know I had is underlying everything and would like to consult with you before going down the road of retraining my tongue/jaw posture in isolation and expecting that to ‘work’. I’ve noticed that the tongue is very compromised on that same side so it is certainly a symptom but trying to put my tongue into correct posture also sets off TOS flare-ups.
I would like to book a consult with you and present you with all the scans you might need to get the full picture. I have 3 year old TMD and entire spine MRIs and a recent dental CBCT scan plus X-rays of the left clavicle as things stand. Enough diagnostic tools for me to bring to a consult? Would that be anything extra that you think would be helpful for you to see based on the rough outline above? Then I can arrange for these before booking and upload relevant scans. Many thanks
Hi, yes.
Hi Kjetil, thanks for writing this comprehensive article!
Assuming a patient with costoclavicular nTOS and several(5-7) years of sensory symptoms only, what time frame of recovery on average would you expect/advise the patient after starting to implement the advocated steps in the article?
Keep up the great work!
It’s not that simple because there are so many things that you can do wrong. I can only calculate an average based on a certain level of compliance and attention to detail.